Atypical presentation of melorheostosis with soft tissues involvement: a case report (original) (raw)
- Case Report
- Open access
- Published: 20 January 2021
- Juhara Haron1 &
- Nik Fatimah Salwati Nik Malek2
Egyptian Journal of Radiology and Nuclear Medicine volume 52, Article number: 31 (2021)Cite this article
- 2971 Accesses
- 3 Citations
- Metrics details
Abstract
Background
Melorheostosis is a skeletal disorder giving rise to a dripping wax appearance. The exact cause is still unclear, and the diagnosis is always challenging due to its wide differential diagnoses. Soft tissue involvement of melorheostosis has been reported in previous literatures but it is a rare phenomenon.
Case presentation
A 10-year-old child with melorheostosis presented with hematuria. Ultrasonography (USG) identified a cystic lesion in the right hemipelvis adjacent to the urinary bladder which was initially regarded as an ovarian cyst. Computed tomography (CT) confirmed the cystic lesion as a fusiform right internal iliac artery aneurysm, as well as multiple right retroperitoneal and right lower limb capillary hemangiomas with uterine involvement. Hence, the final diagnosis was atypical melorheostosis with vascular malformations. The patient was managed conservatively with Sirolimus therapy for the vascular anomalies.
Conclusion
Albeit the rare involvement of soft tissues, careful search for vascular malformation is recommended in melorheostosis.
Background
Melorheostosis (Leri’s disease) is a rare benign non-hereditary mesenchymal sclerotic bone dysplasia, characterized by regions of dripping wax or flowing candle wax appearance due to cortical hyperostosis. The name was derived from Greek words for limb (μέλος; melos) and flow (ῥέω; rhéō), for its characteristic appearance of flowing hyperostosis [[1](/articles/10.1186/s43055-021-00412-5#ref-CR1 "Bansal A (2008) The dripping candle wax sign. Radiology 246:638–640. https://doi.org/10.1148/radiol.2462050537
")\].The prevalence is about 0.9 cases per million population and there are approximately 400 cases described in the literature [2]. The estimated incidence of melorheostosis is 1 in 1,000,000. Melorheostosis affects men and women in equal proportions with occurrence reported in child and adult populations [3].
Long bones are commonly affected, although it can affect any segment of the bones. It tends to be segmental and unilateral [[4](/articles/10.1186/s43055-021-00412-5#ref-CR4 "Long HT, Li KH, Zhu Y (2009) Case report: severe melorheostosis involving the ipsilateral extremities. Clin Orthop Relat Res 467:2738–2743. https://doi.org/10.1007/s11999-009-0890-y
")\]. Soft tissue involvement is extremely rare with few reported literatures. Treatment is primarily conservative for pain relief. However, the treatment of soft tissue involvement is variable depending on the types of soft tissues component \[[5](/articles/10.1186/s43055-021-00412-5#ref-CR5 "Hasegawa S, Kanda S, Imada H et al (2017) Melorheostosis with recurrent soft-tissue components: a histologically confirmed case. Skeletal Radiol 46:399–404.
https://doi.org/10.1007/s00256-016-2562-9
"), [6](/articles/10.1186/s43055-021-00412-5#ref-CR6 "Adams DM, Trenor CC, Hammill AM et al (2016) Efficacy and safety of sirolimus in the treatment of complicated vascular anomalies. Pediatrics 137.
https://doi.org/10.1542/peds.2015-3257
")\].Case presentation
A 10-year-old girl with an underlying skeletal dysplasia presented with acute hematuria. She had right thigh to calf area swelling with intermittent right lower limb pain and café-au-lait spots since the age of three. She was initially diagnosed with osteogenesis imperfecta until she presented to our treatment center with episodic vaginal bleeding when she was 6 years old, which was thought to be precocious puberty. Hence, a diagnosis of McCune-Albright syndrome was made due to precocious puberty, café au lait spots, and skeletal dysplasia. A transabdominal USG was performed by the gynecologist who revealed a right ovarian cyst.
On physical examination, there was a right knee fixed deformity with swelling of right thigh and calf, as well as patchy cutaneous dark spots. Per speculum examination was unremarkable. Her laboratory results for thyroid function, erythrocyte sedimentation rate (ESR), rheumatoid factor, luteinizing hormone (LH), follicle-stimulating hormone (FSH), estradiol, serum complements, serum cortisol, serum calcium, serum lactate dehydrogenase (LDH), growth hormone, serum prolactin, and antistreptolysin-O titer (ASOT) are within normal limits. Plain radiographs showed multiple sclerotic cortical hyperostosis with dripping candle wax appearance over the right ilium, T12 vertebra with hypoplastic right 12th rib, right ribs, right femur, right tibia and fibula, right 2nd-5th metatarsal, and right cuboid (Figs. 1 and 2), right scapula, right humerus, right radius, and right hand. Transabdominal USG showed a small right ovarian cyst and thickened urinary bladder wall with blood clots in the urinary bladder. She was referred to the pediatric surgical team for cystitis and to exclude rhabdomyosarcoma.
Fig. 1
Flowing candle wax appearance at the right ilium (big arrow) and T12 vertebra (asterisk) with hypoplastic right 12th rib (arrowhead) on plain radiograph
Fig. 2
Lateral plain radiograph of right tibia and fibula (a) and dorsal oblique of right foot (b) show sclerotic cortical changes of tibia and calcaneum (big arrows), cuboid (arrowhead), and 3rd-5th metatarsal bones (small arrows)
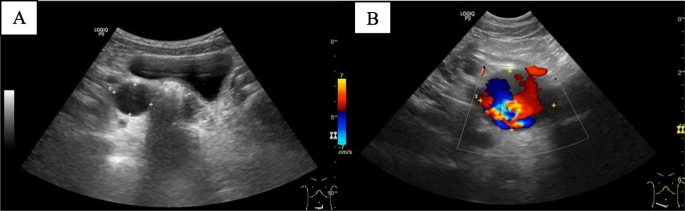
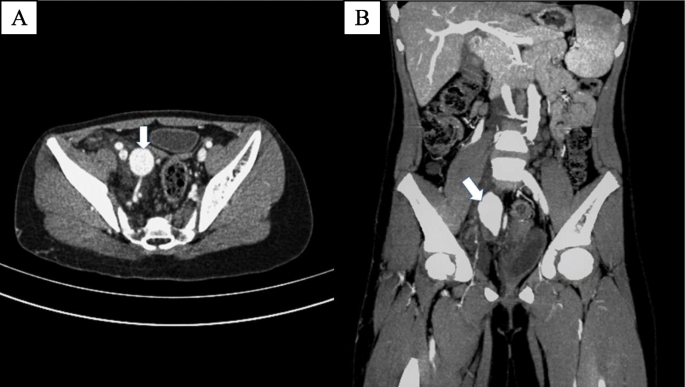
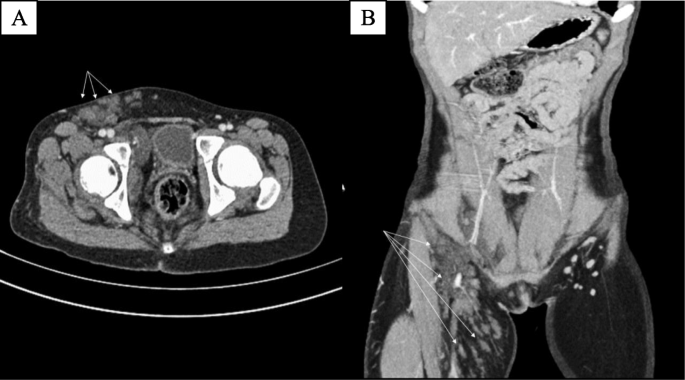
A repeated transabdominal USG by a consultant radiologist revealed a right internal iliac artery aneurysm, which was mistaken as an ovarian cyst (Fig. 3). USG of the right thigh showed thickened echogenic subcutaneous fat with low-flow vascular malformation extending from the right inguinal region till the lower leg. CT angiography of lower limbs confirmed the right internal iliac artery fusiform aneurysm with vascular malformations extending from retroperitoneum to right lower limb with uterine involvement, likely capillary hemangiomas (Figs. 4 and 5). There was no evidence of aneurysm-ureteric fistula. Hence, the final diagnosis was consistent with atypical melorheostosis with vascular malformations. She was treated conservatively with Sirolimus for the vascular malformations.
Fig. 3
Ultrasound of the pelvis shows cystic lesion in right hemipelvis (a). Turbulent flow on color Doppler within the cystic lesion (b)
Fig. 4
Axial (a) and coronal (b) enhanced CT of abdomen and pelvis in the arterial phase demonstrate a fusiform aneurysm (arrow) of the proximal right internal iliac artery
Fig. 5
Axial (a) and coronal (b) enhanced CT of abdomen and pelvis in the arterial phase demonstrate multiple enhancing subcutaneous lesions (small arrows) extending from retroperitoneum to visualized upper thigh suggestive of capillary hemangiomas
Discussion
Melorheostosis or Leri’s disease was first described in 1922 by Leri and Joanny [7]. It was previously hypothesized that melorheostosis was caused by somatic mutations in LEMD3 that is only present in the affected tissues [[8](/articles/10.1186/s43055-021-00412-5#ref-CR8 "Hellemans J, Preobrazhenska O, Willaert A et al (2004) Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet 36:1213–1218. https://doi.org/10.1038/ng1453
")\]. However, recent discovery in molecular biology had identified the causes of melorheostosis. Kang et al. described somatic mosaicism for MAP2K1-activating mutations and SMAD3 mutations as the causes for the classical “dripping candle wax” appearance in melorheostosis \[[9](/articles/10.1186/s43055-021-00412-5#ref-CR9 "Kang H, Jha S, Deng Z et al (2018) Somatic activating mutations in MAP2K1 cause melorheostosis. Nat Commun 9:1390.
https://doi.org/10.1038/s41467-018-03720-z
"), [10](/articles/10.1186/s43055-021-00412-5#ref-CR10 "Kang H, Jha S, Ivovic A et al (2020) Somatic SMAD3-activating mutations cause melorheostosis by up-regulating the TGF-β/SMAD pathway. J Exp Med 217.
https://doi.org/10.1084/jem.20191499
")\].A wide spectrum of soft tissue involvement in melorheostosis was reported in previous literatures, including subcutaneous fibrosis, erythema, linear scleroderma-like patches, ectopic bone formation, hypertrichosis, fibromas, fibrolipomas, and vascular malformations (e.g., capillary hemangiomas, lymphangiectasia, or arterial aneurysms). Soft tissue fibrosis with ligament and tendon retraction had been reported, manifesting as equinovarus or valgus or varus foot deformities. Early presentation and multiple limb involvement may predict a poorer prognosis in terms of complications [[11](/articles/10.1186/s43055-021-00412-5#ref-CR11 "Kotwal A, Clarke BL (2017) Melorheostosis: a rare sclerosing bone dysplasia. Curr Osteoporos Rep 15:335–342. https://doi.org/10.1007/s11914-017-0375-y
")\].Patients with melorheostosis may remain asymptomatic until late adolescence or early adulthood, though changes usually manifest in childhood. Main presenting symptom is often pain worsened by movements of the affected limb [[1](/articles/10.1186/s43055-021-00412-5#ref-CR1 "Bansal A (2008) The dripping candle wax sign. Radiology 246:638–640. https://doi.org/10.1148/radiol.2462050537
")\]. The onset of symptoms in our case started in early childhood with an atypical presentation of episodic vaginal bleeding. Distribution of bone lesions can be monomelic or hemimelic, with the former being the most common observation. It can also be monostotic or polyostotic, and occasionally bilateral involvement \[[12](/articles/10.1186/s43055-021-00412-5#ref-CR12 "Nuño C, Heili Frades Zimmermann SB, Alonso J et al (2001) Melorreostosis: presentación de un caso y revisión de la literatura. Rev Española Enfermedades Metabólicas Oseas 10(2):50–55 ISSN-e 1132-8460")\]. In polyostotic involvement, bone lesions typically cross joint spaces with a sclerotomal distribution. Whyte reported that limb length discrepancy may develop due to asymmetric early epiphyseal fusion \[[13](/articles/10.1186/s43055-021-00412-5#ref-CR13 "Whyte M. “Osteonecrosis, osteosclerosis/hyperostosis, and other disorders of bone”. Goldman's Cecil Medicine: Twenty Fourth Edition. Elsevier Inc; 2011. p. 1605-10.
https://www.elsevier.com/books/goldmans-cecil-medicine/9781437716047
.")\]. We did not observe limb length discrepancy in our patient. Our patient experienced intermittent bone pain, predominantly in the right thigh. The skeletal lesions were distributed in a hemimelic-polyostotic fashion.The soft tissue involvement in our case was vascular malformations and joint contracture of the right knee due to fibrosis. The right internal iliac artery fusiform aneurysm and capillary hemangiomas extending from retroperitoneum to the right lower limb with uterine involvement, explaining the occurrence of episodic vaginal bleeding. The capillary hemangiomas were mistaken for café-au-lait spots, which lead to the initial diagnosis of McCune-Albright syndrome.
Melorheostosis is classically diagnosed using plain radiograph with the pathognomonic appearance of “dripping candle wax or flowing candle wax” appearance due to cortical hyperostosis. CT and MRI may help to identify and delineate the extent of soft tissue involvement. Bone scan may show increased radiotracer uptake in the osseous lesions, albeit plain radiograph is sufficient for the diagnosis of osseous involvement. Serum calcium, serum phosphorus, and alkaline phosphatase are often normal [[11](/articles/10.1186/s43055-021-00412-5#ref-CR11 "Kotwal A, Clarke BL (2017) Melorheostosis: a rare sclerosing bone dysplasia. Curr Osteoporos Rep 15:335–342. https://doi.org/10.1007/s11914-017-0375-y
"), [14](/articles/10.1186/s43055-021-00412-5#ref-CR14 "Teoh CC, Teoh SRZ, Chieng DCH et al (2019) Polyostotic melorheostosis: approach to clinical evaluation and management. Open J Orthop 09:137–144.
https://doi.org/10.4236/ojo.2019.97014
")\]. In our case, the blood results were within normal limit. Histopathologically, findings are nonspecific and often show a mixture of mature and immature bone in a dense formation with increased trabecular bone \[[3](/articles/10.1186/s43055-021-00412-5#ref-CR3 "Alpoim BP, Rodrigues MEGR, Félix AJM et al (2013) Melorheostosis: a case report. Rev Bras Ortop 48:282–285")\].Treatment is conservative for pain alleviation and physiotherapy although in severe cases, surgical intervention may be required, including tendon release, osteotomies, and even amputation. A recent study found that melorheostosis can be treated with intravenous zoledronic acid and that treatment can be monitored by using a specific bone resorption marker [[15](/articles/10.1186/s43055-021-00412-5#ref-CR15 "Hollick RJ, Black A, Reid D (2010) Melorheostosis and its treatment with intravenous zoledronic acid. BMJ Case Rep 2010:bcr0420091757. https://doi.org/10.1136/bcr.04.2009.1757
")\]. Sirolimus can be used to treat vascular malformation with proven safety and efficacy \[[6](/articles/10.1186/s43055-021-00412-5#ref-CR6 "Adams DM, Trenor CC, Hammill AM et al (2016) Efficacy and safety of sirolimus in the treatment of complicated vascular anomalies. Pediatrics 137.
https://doi.org/10.1542/peds.2015-3257
")\].The differential diagnoses include osteopoikilosis, Buschke-Ollendorff syndrome, osteopathia striata, McCune-Albright syndrome, infantile cortical hyperostosis (Caffey disease), and desmoid tumors [16].
Conclusion
Albeit the rare involvement of soft tissue components, careful search for vascular malformation is recommended in melorheostosis. Early identification of soft tissue involvement in melorheostosis may prevent disastrous complications. Sirolimus is proven safe and efficacious in the treatment of vascular anomalies. However, interventional radiology may offer help in the case of complicated vascular malformation, resistant to pharmacotherapy.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
USG:
Ultrasonography
CT:
Computed tomography
MRI:
Magnetic resonance imaging
ESR:
Erythrocyte sedimentation rate
LH:
Luteinizing hormone
FSH:
Follicle-stimulating hormone
LDH:
L_actate dehydrogenase_
ASOT :
Antistreptolysin-O titer
References
- Bansal A (2008) The dripping candle wax sign. Radiology 246:638–640. https://doi.org/10.1148/radiol.2462050537
Article PubMed Google Scholar - Clifford PD, Jose J (2009) Melorheostosis. Am J Orthop (Belle Mead NJ) 38:360–361
Google Scholar - Alpoim BP, Rodrigues MEGR, Félix AJM et al (2013) Melorheostosis: a case report. Rev Bras Ortop 48:282–285
Article Google Scholar - Long HT, Li KH, Zhu Y (2009) Case report: severe melorheostosis involving the ipsilateral extremities. Clin Orthop Relat Res 467:2738–2743. https://doi.org/10.1007/s11999-009-0890-y
Article PubMed PubMed Central Google Scholar - Hasegawa S, Kanda S, Imada H et al (2017) Melorheostosis with recurrent soft-tissue components: a histologically confirmed case. Skeletal Radiol 46:399–404. https://doi.org/10.1007/s00256-016-2562-9
Article PubMed Google Scholar - Adams DM, Trenor CC, Hammill AM et al (2016) Efficacy and safety of sirolimus in the treatment of complicated vascular anomalies. Pediatrics 137. https://doi.org/10.1542/peds.2015-3257
- Leri A (1922) Une affection non decrite des os. Hyperostose “en coulee” sur toute la longueur d’un membre ou “melorheostose”. Bull Mem Soc Med Hop Paris 46:1141–1145
Google Scholar - Hellemans J, Preobrazhenska O, Willaert A et al (2004) Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet 36:1213–1218. https://doi.org/10.1038/ng1453
Article CAS PubMed Google Scholar - Kang H, Jha S, Deng Z et al (2018) Somatic activating mutations in MAP2K1 cause melorheostosis. Nat Commun 9:1390. https://doi.org/10.1038/s41467-018-03720-z
Article CAS PubMed PubMed Central Google Scholar - Kang H, Jha S, Ivovic A et al (2020) Somatic SMAD3-activating mutations cause melorheostosis by up-regulating the TGF-β/SMAD pathway. J Exp Med 217. https://doi.org/10.1084/jem.20191499
- Kotwal A, Clarke BL (2017) Melorheostosis: a rare sclerosing bone dysplasia. Curr Osteoporos Rep 15:335–342. https://doi.org/10.1007/s11914-017-0375-y
Article PubMed Google Scholar - Nuño C, Heili Frades Zimmermann SB, Alonso J et al (2001) Melorreostosis: presentación de un caso y revisión de la literatura. Rev Española Enfermedades Metabólicas Oseas 10(2):50–55 ISSN-e 1132-8460
Google Scholar - Whyte M. “Osteonecrosis, osteosclerosis/hyperostosis, and other disorders of bone”. Goldman's Cecil Medicine: Twenty Fourth Edition. Elsevier Inc; 2011. p. 1605-10. https://www.elsevier.com/books/goldmans-cecil-medicine/9781437716047.
- Teoh CC, Teoh SRZ, Chieng DCH et al (2019) Polyostotic melorheostosis: approach to clinical evaluation and management. Open J Orthop 09:137–144. https://doi.org/10.4236/ojo.2019.97014
Article Google Scholar - Hollick RJ, Black A, Reid D (2010) Melorheostosis and its treatment with intravenous zoledronic acid. BMJ Case Rep 2010:bcr0420091757. https://doi.org/10.1136/bcr.04.2009.1757
Article Google Scholar - Dähnert W (2017) Musculoskeletal system: differential diagnosis of musculoskeletal disorders. In: Radiology review manual, 8th edn. Wolters Kluwer, Philadelphia, pp 46–60
Google Scholar
Author information
Authors and Affiliations
- Department of Radiology, School of Medical Sciences, Universiti Sains Malaysia, Kelantan, Malaysia
Kok King Chia & Juhara Haron - Department of Radiology, Hospital Sultanah Bahiyah, Alor Setar, Kedah, Malaysia
Nik Fatimah Salwati Nik Malek
Authors
- Kok King Chia
- Juhara Haron
- Nik Fatimah Salwati Nik Malek
Contributions
Dr. CKK (1) had made substantial contributions to concept, design, acquisition, interpretation of data, and drafting the article. Dr. NFSNM (3) had made substantial contributions to intellectual content. Dr. JH (2) gave final approval of the version to be submitted. The authors have read and approved the transcript.
Authors’ information
Medical Officer and Radiology Trainee, Department of Radiology, Hospital Universiti Sains Malaysia, 16150 Kota Bharu, Kelantan, Malaysia
Chia Kok King (CKK)
Associate Professor and Consultant Radiologist, Department of Radiology, Hospital Universiti Sains Malaysia, 16150 Kota Bharu, Kelantan, Malaysia
Juhara Haron (JH)
Head of Department and Consultant Radiologist, Department of Radiology, Hospital Sultanah Bahiyah, Km 6, Jalan Langgar, 05460 Alor Setar, Kedah, Malaysia
Nik Fatimah Salwati Nik Malek (NFSNM)
Corresponding author
Correspondence toKok King Chia.
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written consent had been obtained from the parent of study participant.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chia, K., Haron, J. & Nik Malek, N. Atypical presentation of melorheostosis with soft tissues involvement: a case report.Egypt J Radiol Nucl Med 52, 31 (2021). https://doi.org/10.1186/s43055-021-00412-5
- Received: 18 November 2020
- Accepted: 07 January 2021
- Published: 20 January 2021
- DOI: https://doi.org/10.1186/s43055-021-00412-5