The functional and molecular characterisation of human embryonic stem cell-derived insulin-positive cells compared with adult pancreatic beta cells (original) (raw)
Introduction
Type 1 diabetes results from an autoimmune attack on pancreatic beta cells leading to insulin deficiency. Improvements have been made in islet transplantation [1], but problems remain, including low donor numbers and cell loss during islet isolation [2]. The generation of beta cells from human embryonic stem cells (hESCs) could offer an unlimited source of insulin-producing cells for transplantation. Pancreatic cells, including those expressing insulin, can be generated in vitro from hESCs; however, cells develop with low efficiency in heterogeneous cultures, are mostly polyhormonal and have a poorly defined phenotype [3–8]. We hypothesise that understanding the functional nature of in vitro generated endocrine cells and identifying key molecular differences between them and adult beta cells represent important steps towards the generation of functional beta cells suitable for transplantation.
Previously, D’Amour and colleagues generated insulin-producing cells from hESCs (insulin+ cells) using a five-stage differentiation protocol [8]. These insulin+ cells released C-peptide in response to secretagogues, such as KCl; however, they were not glucose-responsive and C-peptide content was ∼50% lower than in human islets, suggesting poor glucose sensing and/or improper insulin processing. More recently, the same group from ViaCyte transplanted hESC-derived pancreatic progenitors (hormone-negative cells) into the fat pads of immunocompromised mice [9]. Maximal insulin secretion occurred 3 months post-implantation, when the mice had plasma human C-peptide levels comparable to those in mice implanted with ∼4,000 human islets. Graft analysis following in vivo differentiation showed that hESC-derived pancreatic progenitors generated beta-like cells that co-produced pancreatic and duodenal homeobox 1 (PDX1), NK6 homeobox 1 (NKX6-1) and insulin independently of other hormones; however, mice became hypoglycaemic during glucose tolerance testing, suggesting that insulin secretion was indiscriminate. In addition, the same hESC-derived pancreatic progenitors transplanted into athymic nude rats failed to produce substantial numbers of beta-like cells [10]. Collectively, this suggests that much progress is still required in the derivation of beta cells from hESC.
We recently developed and characterised a 22-day differentiation protocol that more efficiently generates insulin-producing cells from hESCs [11] (Fig. 1a). The availability of hESCs with green fluorescent protein (GFP) cDNA targeted to the insulin (INS) locus by homologous recombination (INS GFP/w) allowed us to isolate pure insulin+ populations or identify them in mixed cultures (Fig. 1b). Here we have extensively defined the functional, molecular and phenotypic characteristics of day 22-differentiated insulin+ cells compared with murine beta cells and human islets. Although there are differences, a subset of insulin+ cells share many characteristics with mature beta cells, including some insulin-like granules, ion channel activity and intracellular calcium responsiveness, allowing optimism with regard to the generation of fully functioning beta cells in vitro.
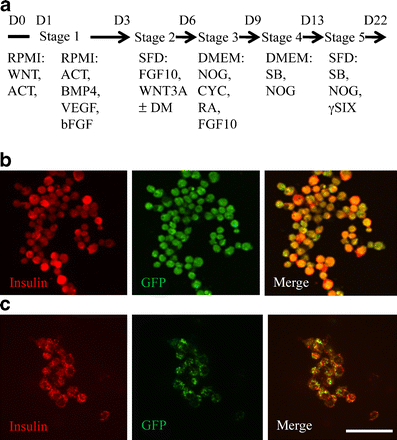
Fig. 1
hESCs were differentiated into insulin+ cells. a The 22 day ‘Nostro protocol’ for hESC differentiation into endocrine cells is divided into five stages; the growth factors, medium and duration of each stage are shown. ACT, activin A; bFGF, basic fibroblast growth factor; BMP4, bone morphogenetic protein 4; CYC, KAAD-cyclopamine; DM, dorsomorphin; FGF10, fibroblast growth factor 10; NOG, noggin; SFD, serum free differentiation media; RA, all-trans retinoic acid; SB, SB 431542; γSIX, γ-secretase inhibitor X, L-685,458; VEGF, vascular endothelial growth factor; WNT, integration 1 wingless. b Immunostaining for insulin in INS:GFP+ cells and (c) in adult murine beta cells isolated from MIP-GFP mice demonstrated 100% co-localisation with GFP. Scale bar, 50 μm
Methods
hESC culture
INS GFP/w and untargeted hESC (HES2) cell lines (ES Cell International, Singapore) approved by the Stem Cell Oversight Committee were differentiated for 22 days using the ‘Nostro protocol’ [11] (Fig. 1a); HES2 cells differentiated for 22 days are referred to as day 22 differentiated HES2 (d22-HES2). Following differentiation, INS GFP/w were FACS-sorted into GFP-producing (INS:GFP+) and GFP-negative (INS:GFP−) fractions [11].
Islet isolation and dispersion
Mouse insulin promoter driving GFP expression (MIP-GFP) mice were a gift from M. Hara (Endocrinology, Diabetes and Metabolism, University of Chicago, Chicago IL, USA). Principles of laboratory animal care were followed and protocols were approved by the University of Toronto Animal Care Committee. Human islets from healthy donors were isolated using the Edmonton protocol [1] and provided by the ABCC Human Islet Distribution Program (University of Alberta, Edmonton AB, Canada). Donation was approved by the local institutional review board. Islets were dispersed as previously described [12].
Immunofluorescent staining
The percentage of mono- and polyhormonal d22-HES2 cells was determined using confocal microscopy and co-localisation software (ImageJ, NIH, Bethesda ML, USA). Cell maturity was determined by expression of immature beta cell markers. The antibodies used are detailed in electronic supplementary material (ESM) Table 1. Staining was performed as previously described [13, 14]. Images were acquired using a confocal microscope (Quorum Wave FX Spinning Disc; Perkin Elmer, Waltham ML, USA) and Volocity software (Perkin Elmer).
Molecular analysis
Microarray
Total RNA was extracted from INS:GFP+ and INS:GFP− fractions, and human islets using a kit (RNeasy mini; Qiagen, Hilden, Germany). Microarray analysis was performed as previously described [15] using the U133_Plus_2.0 Gene Chip (Affymetrix, Santa Clara, CA, USA) at the University Health Network Microarray Centre (Toronto, ON, Canada). Data were summarised and normalised with the robust multi-array method using a software package (Affymetrix Expression Console; Affymetrix). The lowest 20% of robust multi-array values were considered background fluorescence and removed. Significant differences were defined as a twofold or greater change in expression at p < 0.05. Heat maps were generated using the Multi-Experiment Viewer (Dana-Farber Cancer Institute, Boston MA, USA). Hierarchical clustering was performed using Pearson’s correlation with average linkage clustering. Significantly changed genes were functionally classified using the DAVID database and clustered on the basis of GOTERM_MF_2 (http://david.abcc.ncifcrf.gov/, accessed 1 May 2011). Data are compatible with MIAME 2.0 (http://www.mged.org/Workgroups/MIAME/miame.html, accessed 1 May 2011).
Quantitative PCR
Quantitative PCR was performed as previously described [12] on the same samples used for microarray. Primers are listed in ESM Table 2.
Electron microscopy
D22-HES2 cells were fixed and analysed as previously described [16]. Granule morphology was manually quantified [17, 18]. Immunogold staining with insulin and glucagon antibodies (ESM Table 1) was performed on purified INS:GFP+ cells as previously described [19].
Hormone secretion and analysis of the secretion-coupling apparatus
Hormone secretion from d22-HES2 cells or islets was assessed as previously described [12, 17]. Hormone concentrations were measured in the cells and supernatant fraction using a RIA kit (Cedarlane Labs, Burlington, ON, Canada). Electrophysiological analysis of KV, KATP, CaV and Na+ currents in INS:GFP+ (within heterogenous cultures) and islet cells was performed as previously described [12, 20]. Voltage clamp protocols are illustrated in ESM Figs 1–4. Intracellular Ca2+ was measured in INS:GFP_+_ cells and dispersed human islets loaded with Fura2-AM (Molecular Probes, Carlsbad CA, USA) as previously described [12].
Transplantation
Purified INS:GFP+ cells were transplanted into NOD-SCID-γ mice and grafts analysed 1 month later. Details are provided in the ESM Methods.
Statistical analysis
Data are expressed as mean ± SEM. Statistical analysis was performed using a two-tailed student’s t test or ANOVA. Statistical significance was assigned at p < 0.05.
Results
Molecular analysis
We first used transcriptional profiling to characterise the INS:GFP+ cells. Grouped comparisons with INS:GFP− cells were used to determine the commitment of INS:GFP+ cells to an endocrine lineage, while comparison with human islets was used to determine the global relationship of our INS:GFP+ cells with mature endocrine cells (n = 3 per group).
INS:GFP + compared with INS:GFP − cells
Global analysis of INS:GFP_+_ compared with INS:GFP_−_ fractions revealed that 5.8% of genes were changed by two-fold or greater (up- or downregulation, p < 0.05; ESM Fig. 5a). Interestingly, the greatest changes were in genes associated with protein binding, including genes for extracellular matrix proteins (collagens), receptors (IGF1R and GABRB3), proteases (DPP4 and the MMP family), cell cycle proteins (MAD2 [also known as _MAD2L1_] and CCNA2) and cell adhesion proteins (CDH2). To determine endocrine commitment of the INS:GFP+ fraction, 128 genes involved in pancreatic development, metabolism, insulin exocytosis, ion channels and pancreatic hormones [21, 22] were examined (Fig. 2a, b and ESM Fig 6a).
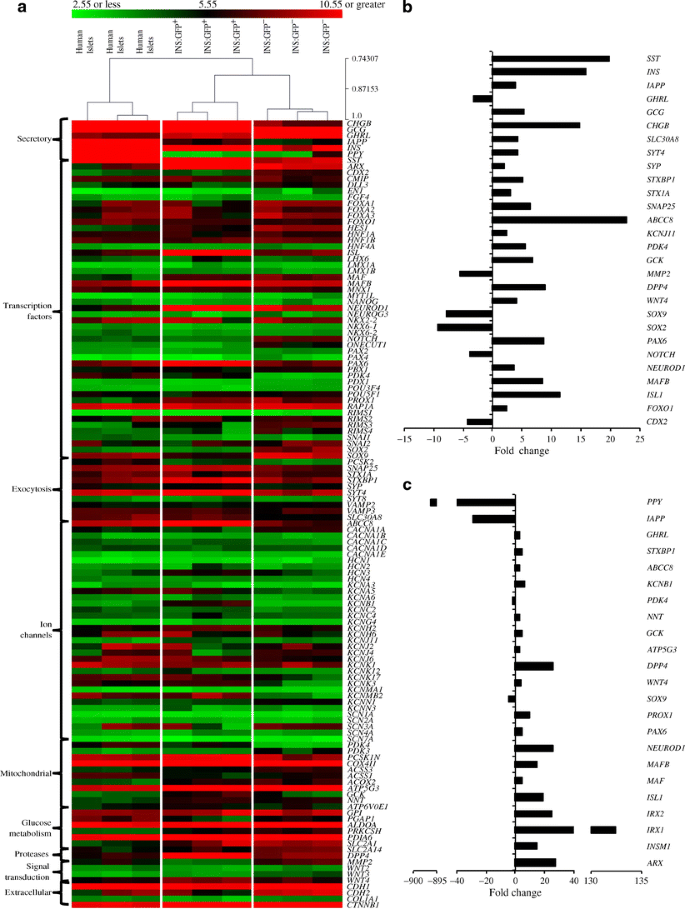
Fig. 2
Expression of genes associated with pancreatic development and islet function with hierarchical cluster analysis. The INS:GFP+ expression profile was compared with INS:GFP− and human islets. a Heat map showing the background-corrected robust multi-array expression values of 128 endocrine lineage genes of interest from three sample sets of human islets, INS:GFP+ and INS:GFP− cells. Hierarchical clustering was determined using Pearson correlation distance metric with average linkage clustering. Of the 128 genes of interest, (b) 28 were significantly changed between the INS:GFP+ and INS:GFP− populations, and (c) 23 were significantly changed between the INS:GFP+ and human islet populations. Significance was defined as a two-fold or greater increased or decreased expression, p ≤ 0.05
The transcriptional regulators NOTCH (also known as NOTCH1), CDX2, SOX2 and SOX9, all of which are involved in early endoderm specification [21, 23], showed higher expression in the INS:GFP− than in the INS:GFP+ fraction (Fig. 2b), whereas transcription factors of the endocrine signature, e.g. NEUROD1, ISL1, MAFB and PAX6 [15, 24], were higher in the INS:GFP_+_ than in the INS:GFP− fraction (Fig. 2b). INS:GFP+ cells expressed more INS than INS:GFP− cells; however, we also observed increased GCG and SST, but reduced GHRL (Fig. 2b). Together, this suggests that the INS:GFP+ fraction more strongly resembled endocrine lineage cells than the INS:GFP− fraction.
To further confirm this, we investigated genes involved in endocrine cell function. KATP channels are expressed in alpha and beta cells, and are required for normal secretory function in both cell types [25]. We examined genes encoding the major subunits of these channels and found increased expression of ABCC8 (protein name SUR1) and KCNJ11 (protein name Kir6.2) in INS:GFP+ compared with INS:GFP− cells (Fig. 2b). Oscillations of Ca2+ levels in endocrine cells are crucial for hormone secretion: in alpha cells N- and P/Q-type Ca2+ channel activity is most important for glucagon release [26], whereas in beta cells, L-type Ca2+ channels predominate [27]. We found levels of the L-type Ca2+ channel CaV1.3 were higher in the INS:GFP+ fraction than in INS:GFP− fraction, with levels of other channel subtypes being similar (ESM Fig. 6a).
Glucokinase is rate-limiting for glucose metabolism in islet cells [28] and expression of its gene was significantly higher in INS:GFP+ than in INS:GFP− cells. A key gene required for insulin biosynthesis and processing, SLC30A8 (also known as ZnT8) [18] was also significantly elevated, along with many components of the exocytotic machinery (SNAP25, STX1A, STXBP1 and SYT4) [29], suggesting an increased capacity for hormone exocytosis. Interestingly, synaptophysin (SYP), an islet surface marker [30], was more highly expressed in the INS:GFP+ than in the INS:GFP− fraction (Fig. 2b and ESM Fig. 6a).
INS:GFP + cells compared with human islets
Global analysis of INS:GFP+ cells compared with human islets revealed that 14.4% of genes were changed by twofold or greater (up- or down-regulation, p < 0.05; ESM Fig. 5b). Approximately 50% of significantly changed genes in the INS:GFP+ fraction encoded proteins involved in protein- or ion-binding. The ion-binding category includes genes involved in ion transport (e.g. Na+/H+ exchangers and K+ channels, including KCNJ11), transcription factors (zinc-finger proteins) and amino acid transporters (SLC7A8). The same 128 genes of interest examined above were compared in INS:GFP+ cells and human islets (Fig. 2a, c and ESM Fig. 6b).
Endoderm specification genes were expressed at similarly low levels in INS:GFP+ cells and human islets, indicating maturity beyond this developmental stage. Expression of a cluster of transcription factors following NGN3 (also known as NEUROG3)-dependent endocrine commitment (NEUROD1, ISL1, PAX6, PROX1 and MAFB) was significantly increased in INS:GFP+ cells compared with human islets, although many, including PAX4, were expressed at similar levels (Fig. 2c and ESM Fig. 6b). Microarray analysis showed that NKX6-1 expression was 1.45-fold lower in INS:GFP+ cells than in human islets, this difference being significant by quantitative PCR (Fig. 2a and ESM Fig. 6b, 7). In addition, the expression of beta cell-specific transcription factors such as INSM1 and MAF were higher in INS:GFP+ cells, while alpha cell lineage transcription factors IRX1 and ARX [30, 31] were also markedly increased. INS, GCG and SST were expressed at the maximum level detectable by microarray in the INS:GFP+ and human islet fractions, while PPY and IAPP expression was lower in INS:GFP+ cells than in human islets (Fig. 2c). Quantitative PCR analysis revealed that INS, GCG and SST expression was in fact significantly lower in the INS:GFP+ fraction than in human islets (ESM Fig. 7), confirming previous reports [11].
Most key ion channel genes were expressed at similar levels to those in human islets, with the exception of ABCC8, KCNJ11 and KCNB1 (higher expression of all three), and SCN3A, which had significantly lower expression (ESM Fig. 6b). The expression of important metabolic and mitochondrial genes, such as GCK, NNT and ATP5G3 [17], was higher in INS:GFP+ cells than in human islets (ESM Fig. 6b). Therefore, while INS:GFP+ and INS:GFP− cells are globally more similar to each other (Fig. 2a), the INS:GFP+ population was more similar to human islets regarding genes involved in endocrine cell development and function.
Immunofluorescent staining
To determine hormone production and cell maturity, we used immunofluorescent staining. Insulin and GFP were completely co-localised in purified INS:GFP+ cells (Fig. 1b). However, d22-HES2 insulin+ cells were often polyhormonal (Fig. 3a). In a heterogeneous population of d22-HES2 cells, 19.77 ± 13.80% (mean ± SEM) were insulin+, 9.3 ± 1.06% were glucagon+ and 7.7 ± 0.4% were somatostatin+ (n = 3 batches of cells, 480 cells total). Cells also co-produced C-peptide and GLUT-2 (Fig. 3a).
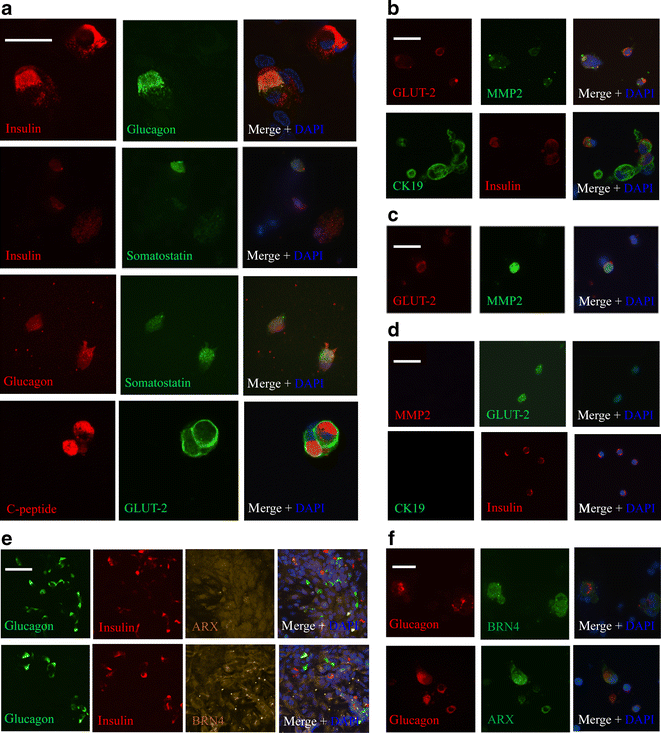
Fig. 3
d22-HES2 cells exhibit a polyhormonal phenotype and markers associated with alpha and beta cells. a Immunostaining for insulin, glucagon, somatostatin, C-peptide and GLUT2 in d22-HES2 cells. Co-localisation was examined with ImageJ software. Results were measured as an intensity correlation quotient (ICQ), where 0.5 shows a complete co-localisation value. ICQ values between insulin and glucagon were 0.387 ± 0.01 (mean ± SEM), between insulin and somatostatin 0.110 ± 0.01, and between glucagon and somatostatin 0.173 ± 0.004. The trans-membrane glucose carrier protein, GLUT-2, and C-peptide are co-produced in d22-HES2 cells. b Immunostaining for immature beta cell markers MMP2, CK19 and GLUT-2 showed that d22-HES2 cells produce MMP2 (with GLUT-2) and CK19 (with insulin). c Staining as indicated in (b) in P1 murine dispersed islets and (d) in adult murine dispersed islet cells, showing that the latter no longer produce MMP2 or CK19. e Immunostaining for ARX and BRN4 in d22-HES2 cells and (f) in adult murine alpha cells. Scale bars (a–e) 50 μm, (f) 15 μm
To assess the degree of d22-HES2 cell maturity, we examined the presence of the immature beta cell markers matrix metallopeptidase 2 (gelatinase A, 72 kDa gelatinase or type IV collagenase) (MMP2), a neutral endopeptidase that cleaves most extracellular matrix proteins and is important in islet formation [32, 33], and cytokeratin 19 (CK19), an intermediate filament protein that is found in the basal epidermis and is indicative of cells in a flexible state of differentiation [33]. MMP2 and CK19 were present in d22-HES2 cells (Fig. 3b) and in murine islets at postnatal day 1 (P1) (Fig. 3c), but not in adult murine beta cells (Fig. 3d), suggesting that d22-HES2 cells have an immature endocrine phenotype [33]. The alpha cell-specific transcription factors, aristaless related homeobox (ARX) and brain-specific homeobox/POU domain protein 4 (BRN4), co-localised with insulin−/glucagon+, insulin+/glucagon− and insulin+/glucagon+ d22-HES2 cells (Fig. 3e), and also co-localised with glucagon in adult murine alpha cells (Fig. 3f) (n = 3).
Electron microscopy
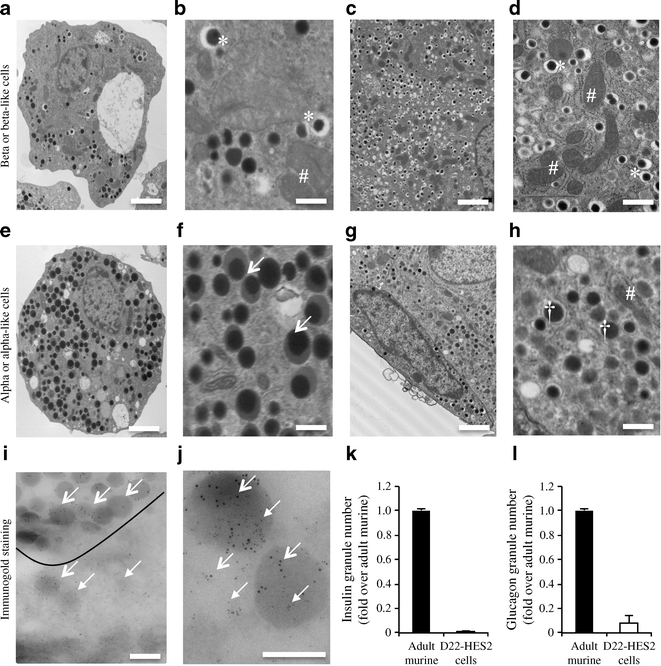
For beta cells to secrete insulin, they must synthesise and package it correctly in secretory granules. The cellular ultrastructure of d22-HES2 cells was examined by electron microscopy and compared with that of murine beta cells. Insulin granules are characterised by a dense black core surrounded by a white halo [34] when fixed using aldehyde [35] (Fig. 4c, d). d22-HES2 cells had fewer total granules than murine beta cells (Fig. 4a, c, k), and only about 2% of cells contained ‘typical’ insulin granules. Of the cells containing insulin-like granules, only around 12% of all granules displayed the typical morphology; the others were more reminiscent of a glucagon granule, containing a dense black or grey core without a halo [30] (Fig. 4a, b). Another 2% of all d22-HES2 cells contained unusual granules with a dense black core surrounded by a grey halo (18% of all granules in this cell type) (Fig. 4e, f). The remaining 96% of d22-HES2 cells contained only granules without a halo which are more like murine alpha cell granules (Fig. 4g, h). The granule number was much lower in d22-HES2 cells than in murine beta cells, with 100-times fewer insulin-like granules (Fig. 4k) and 12.5-times fewer glucagon-like granules (Fig. 4l) in the former. Consistent with an islet cell phenotype, and due to their role in glucose metabolism, all cells with typical insulin granules had many mitochondria (Fig. 4b, d, h).
Fig. 4
Electron microscopy revealed that some d22-HES2 and purified INS:GFP+ cells contain insulin granules. a The typical insulin granules can be recognised by their dense black core surrounded by a white halo. b d22-HES2 cells contained some granules with no halo and some exhibited insulin granule morphology. The cells also contain large numbers of mitochondria. a Image at low magnification, scale bar 2 μm, and (b) at high magnification, scale bar 500 nm. c Murine beta cells showing normal mitochondria and insulin granules, scale bar 1 μm, and (d) murine beta cells at high magnification, scale bar 500 nm. e Other d22-HES2 cells contained granules with a similar morphology, but the dense black core was surrounded by a grey halo. These cells also had fewer mitochondria than beta or alpha cells. Image is at low magnification, scale bar 2 μm, and (f) at high magnification, scale bar 500 nm. g Murine alpha cell with grey glucagon granules. There are no examples of the grey halo granule morphology. Scale bar 1 μm. h Murine alpha cell at high magnification, scale bar 500 nm. a–h Asterisks (*), dense core (insulin) granules; arrows, grey halo granules; dagger symbols (†), glucagon granules; hash symbols (#), mitochondria. i Immunogold labelling revealed that some INS:GFP+ cells produce only insulin (10 nm gold particles, open head arrows), while some produce insulin and glucagon (6 nm particles, closed head arrows), scale bar 500 nm. j In bi-hormonal INS:GFP+ cells insulin (open head arrows) and glucagon (closed head arrows) are also found in the cytoplasm, scale bar 500 nm. k, l The granule number was much lower in d22-HES2 cells than in murine islet cells; there were 100 times fewer typical insulin granules (k) and 12.5 times fewer typical glucagon granules (l)
Immunogold labelling of purified INS:GFP+ cells revealed that 24.5 ± 10% of granules were insulin+, 33.0 ± 11% glucagon+ and 35.0 ± 12% insulin- and glucagon-positive, while 7.5 ± 1% contained neither insulin nor glucagon (Fig. 4i). Cytosolic hormone production was also observed, with 10 ± 10% containing cytosolic insulin, 20 ± 13% glucagon and 50 ± 17% both (n = 3) (Fig. 4j).
Hormone secretion
The hallmark of a mature beta cell is its ability to secrete insulin in response to high glucose, so it was very important to determine the glucose responsiveness of d22-HES2 cells. In all cases, human and murine islets secreted insulin in response to high glucose and direct cellular depolarisation (30 mmol/l KCl) (Fig. 5a, b and ESM Tables 3 and 4). However, d22-HES2 cells only secreted insulin consistently under direct cellular depolarisation and did not respond to glucose (Fig. 5c and ESM Table 5). During this depolarisation-induced secretion, d22-HES2 cells secreted approximately 1.5-fold less insulin than human islets, i.e. 3.541 (±1.40) and 5.16 ± 0.82 ng/μg DNA respectively. However, this was not significant (ESM Tables 3 and 5). Moreover, d22-HES2 cells contained approximately five-fold less total insulin than human islets, i.e.: 496.79 ± 0.04 vs 2,221.0 ± 904.35 ng insulin/μg DNA, respectively (p < 0.05).
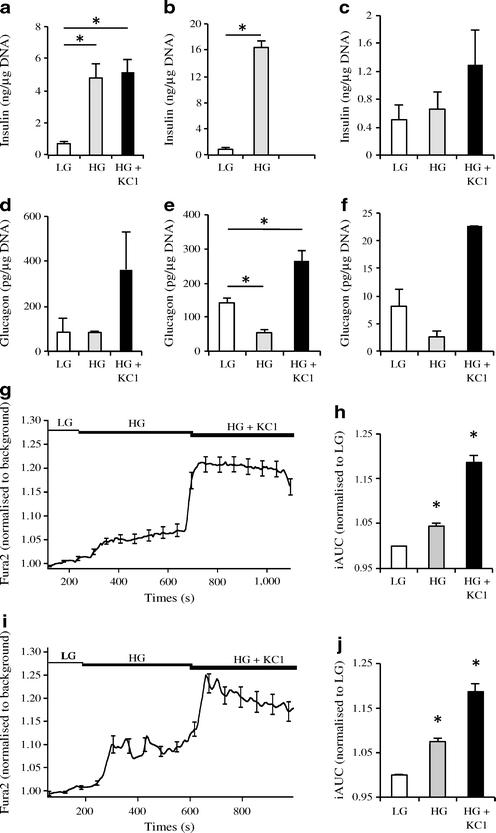
Fig. 5
Insulin+ hESCs do not secrete hormones in response to high glucose but do increase their intracellular calcium levels half of the time. a Representative insulin secretion from human islets, (b) murine islets and (c) d22-HES2 cells. d–f Representative glucagon secretion from the same cell groups. a In all experiments human islets secreted insulin in response to high glucose (HG: 20 mmol/l) (grey bars) and glucose plus direct depolarisation (HG + KCl: 30 mmol/l KCl) (black bars). White bars, low glucose (LG: 1 mmol/l). b Murine islets secreted insulin in response to HG. c All d22-HES2 cells secreted insulin due to cell direct depolarisation (HG + KCl), but did not respond to HG. d Human islets secreted glucagon in response to cellular depolarisation (HG + KCl). e Murine islets secreted glucagon in response to LG and direct cellular depolarisation (HG + KCl), and (f) d22-HES2 cells secreted glucagon in all experiments due to direct depolarisation (HG + KCl). In five batches (f) cells were also responsive to LG. a–f Hormone secretion was normalised to total DNA content. Raw data can be found in ESM Tables 3–5. Representative results are shown; n = 11. *p < 0.05. g, h Cytosolic Ca2+ flux in INS:GFP+ cells and (i, j) human islet cells in response to glucose and cellular depolarisation with 30 mmol/l KCl. g Average of responses from all INS:GFP+ cells, with (h) the average incremental AUC (iAUC) for all cells, normalised to the LG values; n = 42, in three cell batches. HG, high glucose. i Average of responses from all dispersed human islet cells, with (j) bar graph showing the average incremental AUC for all cells, normalised to the LG values; n = 45, cells from three cell batches. Horizontal bars (g, i) represent perifusion with the corresponding reagents; error bars represent ± SEM; *p < 0.05
In contrast to insulin secretion, d22-HES2 cells secreted glucagon in response to direct depolarisation (30 mmol/l KCl) and half the time also responded to low glucose (Fig. 5f and ESM Table 5) similarly to human and murine islets (Fig. 5d, e and ESM Tables 3 and 4). The d22-HES2 cells secreted approximately 4.4-fold less glucagon than human islets, i.e. 28.74 ± 17.89 versus 123.17 ± 19.41 pg/μg DNA, respectively (p < 0.05) (ESM Tables 3 and 5). Total glucagon content was approximately 146-fold lower in d22-HES2 cells than in human islets, i.e. 172.56 ± 32.92 vs 25,218.41 ± 7,527.25 pg/μg DNA, respectively (n = 3, p < 0.05). Collectively, this supports the observation by transmission electron microscopy that INS:GFP+ cells had fewer granules.
Ca2+ uptake
To provide a more in-depth mechanism linking glucose metabolism to insulin secretion, cytosolic Ca2+ flux, which mirrors cellular electrical activity and biphasic insulin secretion [12], was measured. In 81% of purified INS:GFP+ cells we observed increased levels of intracellular Ca2+ during cellular depolarisation (30 mmol/l KCl); these increases were similar to those in human islet cells (Fig. 5g–j). Interestingly, 57% of INS:GFP+ cells responded to high glucose (significant difference in the incremental AUC) (ESM Fig. 8), indicating that a subset of INS:GFP+ cells were able to increase cytosolic Ca2+ similarly to human islet cells (Fig. 5g, h); however, this did not translate into glucose-induced insulin secretion (n = 3).
Electrophysiology
Since hormone secretion and Ca2+ uptake are dependent on ion channel activity, we examined the electrogenic response. Following KATP channel closure and cellular depolarisation, L-type Ca2+ channels open allowing Ca2+ entry and insulin exocytosis, before activation of KV channels repolarise the cell to its resting state [36].
Whole-cell recordings revealed KATP currents in human islet cells. However, such currents were not consistently observed in INS:GFP+ cells. Individual cell traces are shown in ESM Fig 1a. The KATP channel activator diazoxide (100 μmol/l) activated a KATP current in human islet cells (Fig. 6b) and murine beta cells (ESM Fig. 4a) that was blocked by application of the KATP channel-specific blocker, tolbutamide. A similar response was observed in five of 11 (45.5%) INS:GFP+ cells (Fig. 6a), whereas the remaining six did not respond (ESM Fig. 3). Whole-cell KATP current recordings were also collected in P1 murine beta cells (ESM Fig. 2b) as a control and showed that blockage occurred upon tolbutamide application.
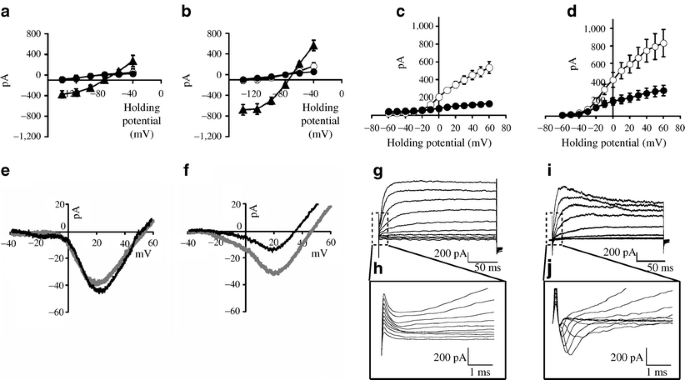
Fig. 6
Whole cell recordings of KATP, CaV, Na+ and KV currents in dispersed INS:GFP cells and human islet cells. Average I/V curves in (a) INS:GFP+ cells and (b) human islet cells were obtained by measuring the maximum current and plotting these against the applied potential (n = 5 for each). Black circles, tolbutamide; triangles, diazoxide; white circles, KATP current recordings at rest (control). In human islet cells (b), diazoxide (100 μmol/l) application produced a large KATP current that was blocked by tolbutamide 250 μmol/l. KV current recordings in (c) INS:GFP+ cells (n = 3), and (d) human islet cells (n = 7). Average I/V curves were obtained by measuring the maximum current and plotting these against the applied potential. White circles, control; black circles, TEA. Representative CaV current recordings in (e) INS:GFP+ cells and (f) human islet cells in response to a voltage ramp. In six of 14 INS:GFP+ cells a CaV current was present (control, grey line), but not blocked by nifedipine (10 μmol/l) (black line), whereas in human islet cells (f) nifedipine decreased the CaV current (n = 6). Representative whole cell current recordings of Na+ current in (g, h) INS:GFP+ cells and (i, j) in human islet cells. The early time scale (dashed line boxes in g and i) was enlarged and is shown separately. g, h INS:GFP+ cells held at −120 mV did not show any voltage‐gated Na+ current (n = 7). i, j Dispersed human islet cells held at −120 mV displayed a voltage-gated Na+ current (n = 6)
Whole-cell recordings showed KV currents in all INS:GFP+ cells; these currents were substantially reduced by the delayed rectifier KV current blocker, tetra-ethyl ammonium (TEA, 20 mmol/l; Fig. 6c). Individual cell traces are shown in ESM Fig. 1b. Control KV recordings were also collected in dispersed human islet cells (Fig. 6d), and in P1 and murine beta cells (ESM Figs 2a and 4d) with similar TEA inhibition.
Whole-cell Ca2+ current recordings were examined in human islet cells and INS:GFP+ cells with a ramp stimulation protocol applied at 0.47 mV/ms to prevent activation of voltage-gated Na+ channels. Nifedipine (L-type CaV channel blocker) decreased the Ca2+ current in human islet cells (Fig. 6f), whereas the INS:GFP+ cells displayed a nifedipine-resistant Ca2+ current in six of 14 cells (42%) (Fig. 6e).
When human islet cells (Fig. 6i–j) and murine beta cells (ESM Fig. 4c) were held at a potential of −120 mV and stimulated with a protocol similar to the one used to record KV, a fast inward Na+ current was detected. The same protocol used on INS:GFP+ cells did not show any voltage gated Na+ current (n = 3) (Fig. 6g–h).
Developmental potential
To evaluate the developmental potential of INS:GFP+ cells, FACS-sorted cells were transplanted into the mammary fat pad of NOD-SCID-γ mice (n = 3). Graft analysis 1 month post transplant revealed a homogeneous population of glucagon-positive, insulin-negative cells. For more details, see ESM text and ESM Fig. 9.
Discussion
The ‘Nostro protocol’ [11] consistently generated insulin+ cells in vitro from the INS GFP/w reporter line and a HES2 line. The use of hESC-derived INS:GFP+ cells enabled us to correlate the results of gene expression with electrophysiological and ultrastructural studies of purified insulin+ cells. End-stage cells were often polyhormonal, with presence of markers such as MMP2 and CK19, which are characteristic of immature pancreatic cells. Immunogold staining of INS:GFP+ cells confirmed the presence of defined insulin [18] and glucagon granules [30], many bi-hormonal granules, and some cytosolic insulin and glucagon. INS:GFP+ cells exhibited KATP and nifedipine-resistant CaV currents half the time, and lacked Na+ currents. Critically, we showed key molecular and functional differences between hESC-derived insulin+ cells and human beta cells, despite many striking similarities.
Glucose-regulated insulin secretion, the hallmark of a mature beta cell, still eludes us, as the hESC-derived insulin+ cells generated in vitro only secreted insulin following membrane depolarisation. The amount of secreted and intracellular insulin was 1.5- to 5-fold lower in the current iteration of differentiated hESCs than in human islets per μg DNA. However, if the relative ratios of insulin+ cells in the d22-HES2 cultures (∼20%) and in human islets (∼80%) are considered, then the insulin+ cells actually secrete similar amounts of insulin per cell under membrane depolarisation. The lack of glucose-responsive insulin release suggests that the INS:GFP+ cells have a deficiency in glucose-sensing, metabolism, insulin processing and/or exocytosis. Molecular analysis showed no difference in GLUT-1, the primary transporter of glucose into human beta cells [37]. The key glycolytic gene GCK and numerous genes involved in mitochondrial metabolism of glucose and generation of ATP, such as NNT and ATP synthase subunits, were more highly expressed in INS:GFP+ cells than in human islets, suggesting that there are no obvious metabolic deficiencies (ESM Fig. 10b). Collectively, this implies that INS:GFP+ cells have sufficient expression of genes involved in glucose-sensing and metabolism, but are still in an immature, polyhormonal state that limits their glucose responsiveness.
Ion channels link beta cell glucose sensing to insulin secretion. D’Amour et al. observed glucose-responsive C-peptide release from hESC-derived endocrine cells only 10% of the time. They confirmed the presence of the KATP channel genes ABCC8 and KCNJ11 by PCR, but did not perform electrophysiological analysis [8]. Our studies show that despite KATP channels being more highly expressed in INS:GFP+ cells than in human islets, the channels were active only 45% of the time. In addition, glucose-mediated Ca2+ uptake, which is distal to the KATP channel and required for insulin exocytosis [25], was measured in only 57% of INS:GFP+ cells, with 42% displaying a nifedipine-resistant voltage-dependent Ca2+ current. Collectively, the heterogeneous channel activity supports the lack of glucose-mediated insulin secretion and could be explained by two different scenarios. First, there may be a discrepancy between mRNA expression and protein levels. Second, channels are translated but may not be functional in polyhormonal cells. Previous studies have demonstrated that embryonic and postnatal rodent beta cells are polyhormonal and also poorly responsive to glucose, in part due to reduced levels of key stimulus–secretion coupling proteins, including glucose transporters and CaV channels; they also lack KATP channel activity [38–40]. Although we are unable to compare INS:GFP+ cells with human embryonic beta cells, the above suggests that most hESC-derived insulin+ cells resemble immature endocrine cells, but the subset showing normal channel activity might represent more mature endocrine cells.
Activation of a KV current is required for the regulation of insulin and glucagon secretion [41, 42]. We found that KV channels were functionally present in all INS:GFP+ cells. In addition, KCNB1 expression was significantly higher in INS:GFP+ cells than in human islets as measured by microarray. It is possible that KV channel over-activity in INS:GFP+ cells could hyperpolarise the plasma membrane and limit insulin secretion, especially when glucose is present. Future studies should test this theory, but currently the electrophysiological data suggests that our cells more closely resemble naive endocrine cells than hyperpolarised ones.
While INS:GFP+ and INS:GFP− cells express endodermal markers, INS:GFP− cells show increased expression of non-pancreatic foregut-derivative and neuronal markers (data not shown), suggesting that this fraction is very heterogeneous. Stronger hormone expression in INS:GFP+ cells indicates that they are more endocrine-committed (we predict past murine embryonic day 10.5 or human week 4 [ESM Fig. 10a]). Upregulation of transcription factors required for endocrine specification in INS:GFP+ cells compared with human islets occurred for those expressed following _NGN3_-dependent endocrine commitment and included ISL1, NEUROD1, PAX6 and PROX1. Cells at this stage are often labelled cells of the ‘first’ transition of pancreatic development, which in the mouse embryo do not produce mature beta cells [24]. Instead, cells from the ‘second’ transition of pancreatic development, a well-defined group of hormone+ cells that delaminate from the pancreatic epithelium, are thought to mature into islet cells [43, 44]. This, together with our observation that most, but not all INS:GFP+ cells are polyhormonal and co-express GCG and/or SST suggests they may be misdifferentiated and unable to generate mature beta cells. However, we also observed upregulation of some alpha (ARX, IRX1/2) [30, 31] and beta (MAF and INSM1) [40, 45] cell lineage-specific transcription factors, suggesting that a small proportion of cells might be heading towards a mature endocrine cell phenotype.
High levels of alpha cell-specific transcription factors, glucose-responsive glucagon secretion and transplantation results where the INS:GFP+ cells downregulated insulin expression and expressed only glucagon (ESM Fig. 9) raise the possibility that some insulin+ cells could be becoming functional alpha cells, as was observed by Rezania et al. using H1-derived pancreatic-differentiated cultures [30]. A recent study by Kelly et al. showed that cells transplanted after sorting using a ‘pancreatic endoderm’ surface marker antibody were able to generate monohormonal _INS_-, _GCG_-, and _SST_-expressing cells. However, cells sorted using an ‘endocrine-like’ surface marker antibody, and thus hormone-positive cells, generated only glucagon-producing cells in vivo [46]. Our transplant data, which support these findings that hormone-positive cells become homogeneously glucagon-positive in vivo, raises the possibility that unknown in vivo factor(s) are required to convert pancreatic endodermal cells to beta cells and that this factor is missing in current in vitro protocols. It is also possible that monohormonal insulin+ cells may not survive in vivo and that polyhormonal cells residing in the INS:GFP+ fraction survive and differentiate into alpha cells [47]. However, given the right differentiation conditions [47] or genetic manipulation, it may be possible to increase the percentage of monohormonal hESC-derived insulin+ cells and improve glucose responsiveness.
NKX6-1 is required for beta cell specification and glucose-mediated insulin secretion [48, 49], and its overproduction promotes INS expression while simultaneously suppressing GCG expression [50]. Based on the success of a recent study showing that glucose responsiveness could be induced in postnatal day 2 rat islet cells by transduction of MAF expression [40], we speculate that the addition of key transcription factors such as NKX6-1 could improve the generation of functional insulin+ cells from hESCs. Therefore, future studies will use the genetic profiling and functional data gained in this study to identify potential targets for molecular manipulation during differentiation. This strategy may allow us to produce fully functional pancreatic beta cells in vitro from hESC.
References
- Shapiro AM, Lakey JR, Ryan EA et al (2000) Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med 343:230–238
Article PubMed CAS Google Scholar - Correa-Giannella ML, Raposo do Amaral AS (2009) Pancreatic islet transplantation. Diabetol Metab Syndr 1:9
Article PubMed Google Scholar - Chen S, Borowiak M, Fox JL et al (2009) A small molecule that directs differentiation of human ESCs into the pancreatic lineage. Nat Chem Biol 5:258–265
Article PubMed CAS Google Scholar - Jiang J, Au M, Lu K et al (2007) Generation of insulin-producing islet-like clusters from human embryonic stem cells. Stem Cells 25:1940–1953
Article PubMed CAS Google Scholar - Jiang W, Shi Y, Zhao D et al (2007) In vitro derivation of functional insulin-producing cells from human embryonic stem cells. Cell Res 17:333–344
Article PubMed CAS Google Scholar - Mfopou JK, Chen B, Mateizel I, Sermon K, Bouwens L (2010) Noggin, retinoids, and fibroblast growth factor regulate hepatic or pancreatic fate of human embryonic stem cells. Gastroenterology 138:2233–2245
Article PubMed CAS Google Scholar - Zhang D, Jiang W, Shi Y, Deng H (2009) Generation of pancreatic islet cells from human embryonic stem cells. Sci China C Life Sci 52:615–621
Article PubMed Google Scholar - D'Amour KA, Bang AG, Eliazer S et al (2006) Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells. Nat Biotechnol 24:1392–1401
Article PubMed Google Scholar - Kroon E, Martinson LA, Kadoya K et al (2008) Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol 26:443–452
Article PubMed CAS Google Scholar - Matveyenko AV, Georgia S, Bhushan A, Butler PC (2010) Inconsistent formation and nonfunction of insulin-positive cells from pancreatic endoderm derived from human embryonic stem cells in athymic nude rats. Am J Physiol Endocrinol Metab 299:E713–E720
Article PubMed CAS Google Scholar - Nostro MC, Sarangi F, Ogawa S et al (2011) Stage-specific signaling through TGFbeta family members and WNT regulates patterning and pancreatic specification of human pluripotent stem cells. Development 138:861–871
Article PubMed CAS Google Scholar - Hardy AB, Fox JE, Giglou PR et al (2009) Characterization of Erg K+ channels in alpha- and beta-cells of mouse and human islets. J Biol Chem 284:30441–30452
Article PubMed CAS Google Scholar - Smukler SR, Arntfield ME, Razavi R et al (2011) The adult mouse and human pancreas contain rare multipotent stem cells that express insulin. Cell Stem Cell 8:281–293
Article PubMed CAS Google Scholar - Diao J, Allister EM, Koshkin V et al (2008) UCP2 is highly expressed in pancreatic alpha-cells and influences secretion and survival. Proc Natl Acad Sci USA 105:12057–12062
Article PubMed CAS Google Scholar - Lyttle BM, Li J, Krishnamurthy M et al (2008) Transcription factor expression in the developing human fetal endocrine pancreas. Diabetologia 51:1169–1180
Article PubMed CAS Google Scholar - Nicolson TJ, Bellomo EA, Wijesekara N et al (2009) Insulin storage and glucose homeostasis in mice null for the granule zinc transporter ZnT8 and studies of the type 2 diabetes-associated variants. Diabetes 58:2070–2083
Article PubMed CAS Google Scholar - Lu H, Koshkin V, Allister EM, Gyulkhandanyan AV, Wheeler MB (2010) Molecular and metabolic evidence for mitochondrial defects associated with beta-cell dysfunction in a mouse model of type 2 diabetes. Diabetes 59:448–459
Article PubMed CAS Google Scholar - Wijesekara N, Dai FF, Hardy AB et al (2010) Beta cell-specific Znt8 deletion in mice causes marked defects in insulin processing, crystallisation and secretion. Diabetologia 53:1656–1668
Article PubMed CAS Google Scholar - Tam P, Mahfoud R, Nutikka A et al (2008) Differential intracellular transport and binding of verotoxin 1 and verotoxin 2 to globotriaosylceramide-containing lipid assemblies. J Cell Physiol 216:750–763
Article PubMed CAS Google Scholar - Leung YM, Ahmed I, Sheu L et al (2005) Electrophysiological characterization of pancreatic islet cells in the mouse insulin promoter-green fluorescent protein mouse. Endocrinology 146:4766–4775
Article PubMed CAS Google Scholar - Bonal C, Herrera PL (2008) Genes controlling pancreas ontogeny. Int J Dev Biol 52:823–835
Article PubMed CAS Google Scholar - D'Amour KA, Agulnick AD, Eliazer S, Kelly OG, Kroon E, Baetge EE (2005) Efficient differentiation of human embryonic stem cells to definitive endoderm. Nat Biotechnol 23:1534–1541
Article PubMed Google Scholar - Van Hoof D, D'Amour KA, German MS (2009) Derivation of insulin-producing cells from human embryonic stem cells. Stem Cell Res 3:73–87
Article PubMed Google Scholar - Du A, Hunter CS, Murray J et al (2009) Islet-1 is required for the maturation, proliferation, and survival of the endocrine pancreas. Diabetes 58:2059–2069
Article PubMed CAS Google Scholar - Aguilar-Bryan L, Bryan J, Nakazaki M (2001) Of mice and men: K(ATP) channels and insulin secretion. Recent Prog Horm Res 56:47–68
Article PubMed CAS Google Scholar - Gopel S, Zhang Q, Eliasson L et al (2004) Capacitance measurements of exocytosis in mouse pancreatic alpha-, beta- and delta-cells within intact islets of Langerhans. J Physiol 556:711–726
Article PubMed Google Scholar - Satin LS (2000) Localized calcium influx in pancreatic beta-cells: its significance for Ca2+-dependent insulin secretion from the islets of Langerhans. Endocrine 13:251–262
Article PubMed CAS Google Scholar - Schuit FC (1996) Factors determining the glucose sensitivity and glucose responsiveness of pancreatic beta cells. Horm Res 46:99–106
Article PubMed CAS Google Scholar - Wang Z, Thurmond DC (2009) Mechanisms of biphasic insulin-granule exocytosis—roles of the cytoskeleton, small GTPases and SNARE proteins. J Cell Sci 122:893–903
Article PubMed CAS Google Scholar - Rezania A, Riedel MJ, Wideman RD et al (2010) Production of functional glucagon-secreting alpha cells from human embryonic stem cells. Diabetes 60:239–247
Article PubMed Google Scholar - Petri A, Ahnfelt-Ronne J, Frederiksen KS et al (2006) The effect of neurogenin3 deficiency on pancreatic gene expression in embryonic mice. J Mol Endocrinol 37:301–316
Article PubMed CAS Google Scholar - Pirila E, Ramamurthy NS, Sorsa T, Salo T, Hietanen J, Maisi P (2003) Gelatinase A (MMP-2), collagenase-2 (MMP-8), and laminin-5 gamma2-chain expression in murine inflammatory bowel disease (ulcerative colitis). Dig Dis Sci 48:93–98
Article PubMed Google Scholar - Aye T, Toschi E, Sharma A, Sgroi D, Bonner-Weir S (2010) Identification of markers for newly formed beta-cells in the perinatal period: a time of recognized beta-cell immaturity. J Histochem Cytochem 58:369–376
Article PubMed CAS Google Scholar - Michael J, Carroll R, Swift HH, Steiner DF (1987) Studies on the molecular organization of rat insulin secretory granules. J Biol Chem 262:16531–16535
PubMed CAS Google Scholar - Suckale J, Solimena M (2010) The insulin secretory granule as a signaling hub. Trends Endocrinol Metab 21:599–609
Article PubMed CAS Google Scholar - MacDonald PE, Wheeler MB (2003) Voltage-dependent K(+) channels in pancreatic beta cells: role, regulation and potential as therapeutic targets. Diabetologia 46:1046–1062
Article PubMed CAS Google Scholar - De Vos A, Heimberg H, Quartier E et al (1995) Human and rat beta cells differ in glucose transporter but not in glucokinase gene expression. J Clin Invest 96:2489–2495
Article PubMed Google Scholar - Navarro-Tableros V, Fiordelisio T, Hernandez-Cruz A, Hiriart M (2007) Physiological development of insulin secretion, calcium channels, and GLUT2 expression of pancreatic rat beta-cells. Am J Physiol Endocrinol Metab 292:E1018–E1029
Article PubMed CAS Google Scholar - Rozzo A, Meneghel-Rozzo T, Delakorda SL, Yang SB, Rupnik M (2009) Exocytosis of insulin: in vivo maturation of mouse endocrine pancreas. Ann N Y Acad Sci 1152:53–62
Article PubMed CAS Google Scholar - Aguayo-Mazzucato C, Koh A, El Khattabi I et al (2011) Mafa expression enhances glucose-responsive insulin secretion in neonatal rat beta cells. Diabetologia 54:583–593
Article PubMed CAS Google Scholar - Spigelman AF, Dai X, MacDonald PE (2010) Voltage-dependent K(+) channels are positive regulators of alpha cell action potential generation and glucagon secretion in mice and humans. Diabetologia 53:1917–1926
Article PubMed CAS Google Scholar - MacDonald PE, Wang X, Xia F et al (2003) Antagonism of rat beta-cell voltage-dependent K+ currents by exendin 4 requires dual activation of the cAMP/protein kinase A and phosphatidylinositol 3-kinase signaling pathways. J Biol Chem 278:52446–52453
Article PubMed CAS Google Scholar - Villasenor A, Chong DC, Cleaver O (2008) Biphasic Ngn3 expression in the developing pancreas. Dev Dyn 237:3270–3279
Article PubMed CAS Google Scholar - Herrera PL, Nepote V, Delacour A (2002) Pancreatic cell lineage analyses in mice. Endocrine 19:267–278
Article PubMed CAS Google Scholar - Artner I, Blanchi B, Raum JC et al (2007) MafB is required for islet beta cell maturation. Proc Natl Acad Sci USA 104:3853–3858
Article PubMed CAS Google Scholar - Kelly OG, Chan MY, Martinson LA et al (2011) Cell-surface markers for the isolation of pancreatic cell types derived from human embryonic stem cells. Nat Biotechnol 29:750–756
Article PubMed CAS Google Scholar - Thorel F, Nepote V, Avril I et al (2010) Conversion of adult pancreatic alpha-cells to beta-cells after extreme beta-cell loss. Nature 464:1149–1154
Article PubMed CAS Google Scholar - Habener JF, Kemp DM, Thomas MK (2005) Minireview: transcriptional regulation in pancreatic development. Endocrinology 146:1025–1034
Article PubMed CAS Google Scholar - Gefen-Halevi S, Rachmut IH, Molakandov K et al (2010) NKX6.1 promotes PDX-1-induced liver to pancreatic beta-cells reprogramming. Cell Reprogram 12:655–664
Article PubMed CAS Google Scholar - Gauthier BR, Gosmain Y, Mamin A, Philippe J (2007) The beta-cell specific transcription factor Nkx6.1 inhibits glucagon gene transcription by interfering with Pax6. Biochem J 403:593–601
Article PubMed CAS Google Scholar