Kineret: Side effects, dosage, how to use, uses, price, and more (original) (raw)
Kineret is a brand-name prescription medication. It’s FDA-approved to:
- Reduce the symptoms and slow the progression (worsening) of moderate to severe rheumatoid arthritis (RA)* in adults. Kineret is prescribed if you’ve tried one or more disease-modifying antirheumatic drugs (DMARDs) that haven’t worked well enough. Your doctor will prescribe Kineret alone or with DMARDs. However, they typically will not prescribe it with tumor necrosis factor blockers, a type of DMARD.†
- Treat neonatal-onset multisystem inflammatory disease (NOMID) in adults and children, including infants. NOMID is a specific type of cryopyrin-associated periodic syndrome (CAPS), a group of rare genetic conditions that start at birth.
- Treat deficiency of interleukin-1 receptor antagonist (DIRA) in adults and children, including infants. DIRA is a rare genetic condition that begins at birth.
For more details about these conditions, see the “Kineret uses” section below.
* RA is an autoimmune condition that causes inflammation (swelling) and pain in and around your joints. † TNF blockers are not recommended for use with Kineret due to the increased risk of infection. To learn more about this side effect, see “Side effect details” in the “Kineret side effects” section below.
Drug details
Kineret is a DMARD. Specifically, it belongs to a drug class called interleukin-1 receptor antagonists (IL-1Ra). IL-1Ra is a protein that your body’s immune system makes naturally. Kineret contains the active ingredient anakinra, which is a recombinant (slightly modified) version of the IL-1Ra protein.
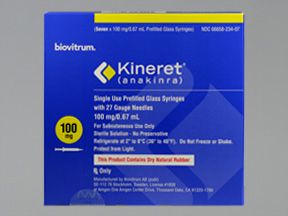
Kineret comes as a solution in a prefilled glass syringe. It comes in one strength: 100 milligrams (mg) in 0.67 milliliters (mL) of solution.
Kineret is given as a subcutaneous injection.
Effectiveness
For information about the effectiveness of Kineret, see the “Kineret uses” section below.
Kineret is available only as a brand-name drug. It’s a biologic medication, which is a drug that’s made from living cells. The active drug of Kineret is anakinra, which is a protein made from E. coli bacteria cells.
Currently, Kineret doesn’t have a biosimilar version. (A biosimilar is a medication that’s similar to a brand-name biologic drug. As with generics, biosimilars tend to cost less than brand-name medications.)
Kineret can cause mild or serious side effects. The drug’s side effects might differ slightly depending on the condition that’s being treated.
The following lists contain some of the key side effects that may occur while taking Kineret. These lists do not include all possible side effects.
For more information about the possible side effects of Kineret, talk with your doctor or pharmacist. They can give you tips on how to manage any side effects that may be concerning or bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs it has approved. If you would like to notify the FDA about a side effect you’ve had with Kineret, you can do so through MedWatch.
Mild side effects
Mild side effects* of Kineret can include:
- headache
- joint pain
- skin rash
- fever
- mild injection site reaction†
- mild infection†
- gastrointestinal (digestive system) side effects†
Most of these side effects may go away within a few days or a couple of weeks. However, if they become more severe or don’t go away, talk with your doctor or pharmacist.
* This is a partial list of mild side effects from Kineret. To learn about other mild side effects, talk with your doctor or pharmacist, or view Kineret’s prescribing information. † For more information about this side effect, see “Side effect details” below.
Serious side effects
Serious side effects from Kineret aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Worsening of rheumatoid arthritis (RA) in people with RA. Symptoms can include:
- Neutropenia (decreased level of neutrophils, a type of white blood cell). This doesn’t directly cause symptoms but may lower your body’s ability to fight infections.
- Severe injection site reaction.*
- Serious infection.*
- Allergic reaction.*
* For more information about this side effect, see “Side effect details” below.
Side effects in children
Kineret is approved to treat the following genetic conditions* in children, including infants:
- neonatal-onset multisystem inflammatory disease (NOMID)
- deficiency of interleukin-1 receptor antagonist (DIRA)
For NOMID, Kineret was studied in infants, children, and adults in clinical trials. The age range was 0.7 years to 46 years. The drug’s most common side effects were similar in all age groups. However, infection was a more common side effect in children under 12 years old.
In clinical trials of Kineret for the treatment of DIRA, researchers studied the drug in children ages 1 month to 9 years. The most common side effects were upper respiratory tract infection, skin rash, fever, and upset stomach.
If you have questions about side effects in children due to Kineret treatment, talk with your child’s doctor. You can also view Kineret’s prescribing information.
* For more information about these conditions, see the “Kineret uses” section below.
Side effect details
Here’s some detail on certain side effects this drug may cause. To find out how often side effects occurred in clinical trials, see the prescribing information for Kineret.
Injection site reaction
Some people may have injection site reactions with Kineret. (Kineret is given as a subcutaneous injection.) Injection site reaction was one of the most common side effects reported in clinical trials of the drug.
Symptoms may include:
- pain or stinging sensation
- redness or discoloration
- swelling
- itchiness
- bruising
- warmth
- bleeding
- lump at the injection site
Injection site reactions are more common when you start Kineret treatment. And symptoms should be temporary. In most cases, injection site reactions from Kineret are mild. However, some people have moderate to severe injection site reactions.
What you can do
To help prevent or lower your risk of injection site reaction, be sure to follow your doctor’s instructions on how to inject Kineret. You can also find instructions in the drug’s patient information. For additional details on how to inject Kineret correctly, see the “How to use Kineret” section below.
Here are some tips to help prevent or ease the symptoms of an injection site reaction:
- Be sure to take the Kineret syringe out of the refrigerator 30 minutes before your injection. Injecting a cold solution can be painful and irritating.
- Place an ice pack or cool compress on the injection site area for a few minutes before and after the injection.
- Apply hydrocortisone or diphenhydramine (Benadryl) cream to the affected areas to ease itchiness.
If your symptoms are bothersome or don’t go away, talk with your doctor. They may want to go over your injection technique with you.
Infection
Some people experience mild or serious infection while receiving Kineret treatment. Mild infections, such as the common cold and upper respiratory infection, were common in the drug’s clinical trials.
Symptoms of infections can vary but generally include:
- runny or stuffy nose
- sore throat
- cough
- sneezing
- fever
- body aches
- fatigue
Treatment with Kineret may increase the risk of developing a serious infection, such as pneumonia, cellulitis, or tuberculosis (TB). This risk is higher in people taking Kineret with drugs that suppress the immune system. Due to this risk, your doctor will not typically prescribe these drugs with Kineret. These include tumor necrosis factor blockers,* such as etanercept (Enbrel).
Certain groups of people may also have an increased risk of infection while taking Kineret. These include adults ages 65 years and older and children under 12 years old.†
* For more information, see the “Kineret interactions” section below. † To learn more, see “Side effects in children” above.
What you can do
If you think you have an infection during Kineret treatment, tell your doctor right away. If you have RA, your doctor may have you stop Kineret treatment until your infection goes away. If you have NOMID or DIRA, your doctor will discuss the risks and benefits of pausing or continuing Kineret treatment.
Gastrointestinal side effects
It’s possible to have gastrointestinal (digestive system) side effects with Kineret treatment. These side effects were commonly seen in clinical trials of Kineret.
Symptoms may include:
- nausea
- diarrhea
- abdominal pain
- vomiting
Gastrointestinal side effects are usually mild and temporary. In severe cases, gastroenteritis may occur with Kineret use. With gastroenteritis, you have inflammation (swelling) or serious infection of the digestive tract.
What you can do
When you first start treatment with Kineret, your doctor may recommend eating smaller meals of bland foods. This may help prevent gastrointestinal side effects from occurring.
If you have diarrhea or vomiting, be sure to drink plenty of fluids to help prevent dehydration. However, if your gastrointestinal side effects don’t go away or become severe, tell your doctor right away.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Kineret. People taking this medication to treat DIRA may have an increased risk of allergic reaction. This risk is higher in the first several weeks of treatment.
Symptoms of a mild allergic reaction can include:
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have an allergic reaction to Kineret, as the reaction could become severe. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
The Kineret dosage your doctor prescribes will depend on several factors. These include:
- the type of condition you’re using Kineret to treat
- your body weight
- other medical conditions you may have, including kidney problems
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
Drug forms and strengths
Kineret comes as a solution in a prefilled glass syringe. It comes in one strength: 100 milligrams (mg) in 0.67 milliliters (mL) of solution.
Kineret is given as a subcutaneous injection. The prefilled syringe is used to inject doses ranging from 20 mg to 100 mg.
Each syringe is meant for one-time use. You’ll discard the syringe after each dose, even if there’s unused medication left in it.
Dosage for rheumatoid arthritis (RA)
The usual dosage of Kineret for RA is 100 mg once daily. Your doctor won’t usually recommend a dose higher than 100 mg.
You should inject your dose at around the same time each day.
If you have kidney problems, your doctor may prescribe a different dosing schedule. Talk with your doctor if you have questions about the dosage that’s right for you.
Dosage for neonatal-onset multisystem inflammatory disease (NOMID)
The usual starting dose of Kineret for NOMID is 1 to 2 mg per kilogram of body weight (mg/kg). (One kilogram is equal to about 2.2 pounds [lb].)
For example, if you weigh 60 kg (about 132 lb), and your doctor prescribed you a 1 mg/kg dose, your total dose would be 60 mg.
If your starting dose isn’t enough to ease your NOMID symptoms, your doctor may increase your dose. They’ll likely increase it in increments of 0.5 to 1 mg/kg up to a maximum of 8 mg/kg.
The recommended dosing schedule of Kineret for NOMID is once daily. Your doctor may recommend splitting your dose into two doses throughout the day.
If you have kidney problems, your doctor may prescribe a different dosing schedule. Talk with your doctor if you have questions about the dosage that’s right for you.
Dosage for deficiency of interleukin-1 receptor antagonist (DIRA)
The usual starting dose of Kineret for DIRA is 1 to 2 mg per kilogram of body weight (mg/kg). (One kilogram is equal to about 2.2 pounds [lb].)
For example, if you weigh 60 kg (about 132 lb), and your doctor prescribed you a 1 mg/kg dose, your total dose would be 60 mg.
If the starting dose isn’t enough to ease your DIRA symptoms, your doctor may increase your dose. They’ll likely increase it in increments of 0.5 to 1 mg/kg up to a maximum of 8 mg/kg.
The recommended dosing schedule of Kineret for DIRA is once daily.
Your doctor may prescribe a different dosing schedule if you have kidney problems. Talk with your doctor if you have questions about the dosage that’s right for you.
Children’s dosages
The following information describes children’s dosages of Kineret that are commonly recommended.
Children’s dosage for neonatal-onset multisystem inflammatory disease (NOMID)
The usual starting dose of Kineret for children with NOMID is 1 to 2 mg per kilogram of body weight (mg/kg). (One kilogram is equal to about 2.2 pounds [lb].)
For example, if your child weighs 20 kg (about 44 lb), and their prescribed dose is 1 mg/kg, their total starting dose would be 20 mg.
If the starting dose isn’t enough to ease the symptoms of your child’s condition, their doctor may increase the dose. They’ll likely increase it in increments of 0.5 to 1 mg/kg up to a maximum of 8 mg/kg.
The recommended dosing schedule of Kineret for NOMID in children is once daily. Your child’s doctor may recommend splitting the dose into two doses throughout the day. Be sure to check with their doctor before splitting their dose.
If your child has kidney problems, their doctor may prescribe a different dosing schedule. Talk with your child’s doctor if you have questions about their dosage.
Children’s dosage for deficiency of interleukin-1 receptor antagonist (DIRA)
The usual starting dose of Kineret for children with DIRA is 1 to 2 mg per kilogram of body weight (mg/kg). (One kilogram is equal to about 2.2 pounds [lb].)
For example, if your child weighs 20 kg (about 44 lb), and their prescribed dose is 1 mg/kg, their total starting dose would be 20 mg.
If the starting dose isn’t enough to ease the symptoms of your child’s condition, their doctor may increase the dose. They’ll likely increase it in increments of 0.5 to 1 mg/kg up to a maximum of 8 mg/kg.
The recommended dosing schedule of Kineret for DIRA in children is once daily.
If your child has kidney problems, their doctor may prescribe a different dosing schedule. Talk with your child’s doctor if you have questions about their dosage.
What if I miss a dose?
If you miss a dose of Kineret, call your doctor. They can tell you when to take your next dose.
To help make sure that you don’t miss a dose, try using a medication reminder. This can include setting an alarm or using a timer. You could also download a reminder app on your phone.
Will I need to use this drug long term?
Most likely, yes. Kineret is meant to be used as a long-term treatment. If you and your doctor determine that Kineret is safe and effective for you, you’ll probably use it long term.
Kineret is administered as a subcutaneous injection. The drug comes with step-by-step instructions for use. However, your doctor or another healthcare professional will first show you or your caregiver how Kineret is administered. Be sure to follow your doctor’s instructions for how to inject Kineret at home. There’s also a helpful video on the manufacturer’s website. You can also refer to Kineret’s patient information for instructions.
You can inject your Kineret dose into the following injection sites:
- the outer area of your upper arms
- the front of your mid-thigh
- the upper outer areas of the buttocks
- the abdomen, avoiding 2 inches around your belly button
Be sure to rotate your injection site. Do not use the same spot every time. Keeping track of the injection site you use may be helpful. You can write it down or make a note on your phone. Or consider using this tracking tool from the drug’s manufacturer.
Avoid injecting Kineret into areas that are swollen, tender, or irritated. Also, be careful not to inject the drug into stretch marks, scars, or veins you can see.
It’s important to notethat each Kineret syringe is meant for one-time use. When you inject your dose, you may not need to use all of the solution in the Kineret syringe. You’ll discard the syringe after each dose, even if there’s unused medication left in it. Your doctor will show you how to prepare the syringe for your prescribed dose. (For more information about dosage, see the “Kineret dosage” section above.)
When to take
There’s no best time of day to administer Kineret. However, you should take your dose at around the same time each day. (The typical dosing of Kineret is once daily.) Be sure to follow the dosing schedule your doctor prescribes for you.
To help make sure that you don’t miss a dose, try using a medication reminder. This can include setting an alarm or using a timer. You could also download a reminder app on your phone.
Accessible labels and containers
If your prescription label is hard to read, talk with your doctor or pharmacist. Some pharmacies offer labels that have large print, braille, or a code you scan with a smartphone to convert text to speech. If your local pharmacy doesn’t have these options, your doctor or pharmacist may be able to direct you to one that does.
The Food and Drug Administration (FDA) approves prescription drugs such as Kineret to treat certain conditions. These are also called indications. Kineret may also be used off-label for other conditions. Off-label drug use is when an FDA-approved drug is prescribed for a purpose other than what it’s approved for.
Kineret for rheumatoid arthritis (RA)
Kineret is approved to reduce the symptoms and slow the progression (worsening) of moderate to severe rheumatoid arthritis (RA) in adults. RA is an autoimmune condition that causes inflammation (swelling) and pain in and around your joints.
Symptoms of RA include:
- joint stiffness
- low-grade fever
- loss of appetite
Kineret is prescribed if you’ve tried one or more disease-modifying antirheumatic drugs (DMARDs) that haven’t worked well enough. (DMARDs are drugs that doctors prescribe to slow the progression of RA.)
Your doctor will prescribe Kineret alone or with DMARDs to treat RA. However, they typically will not prescribe it with tumor necrosis factor (TNF) blockers,* a type of DMARD. TNF blockers are not recommended for use with Kineret due to the increased risk of infection.†
To learn more about managing and treating RA, you can visit _Medical News Today_’s rheumatoid arthritis hub.
Note: The Food and Drug Administration (FDA) hasn’t approved Kineret to treat juvenile RA in children.
* For more information about TNF blockers, see the “Kineret interactions” section below. † To learn more about this side effect, see “Side effect details” in the “Kineret side effects” section above.
Effectiveness for RA
Kineret has been found effective for RA when other treatments haven’t worked well enough. For details on how the drug performed in clinical trials for RA, see Kineret’s prescribing information.
Kineret for neonatal-onset multisystem inflammatory disease (NOMID)
Kineret is used to treat NOMID in adults and children, including infants. NOMID is a specific type of cryopyrin-associated periodic syndrome (CAPS), a group of rare genetic conditions that start at birth.
NOMID causes inflammation (swelling) in the body and related symptoms, such as:
- skin rash that’s present at birth and doesn’t go away
- fever
- chronic meningitis (inflammation of the membrane surrounding the brain), which may cause headaches, vomiting, or seizures
- joint swelling or deformity, particularly around the knees
Effectiveness for NOMID
Kineret has been found effective for treating NOMID in adults and children, including infants. For details on how the drug performed in clinical trials for NOMID, see Kineret’s prescribing information.
Kineret for deficiency of interleukin-1 receptor antagonist (DIRA)
Kineret is approved for use in adults and children with DIRA, a rare genetic condition that begins at birth. With DIRA, a protein called interleukin-1 receptor antagonist (IL-1Ra) doesn’t work as it should. Without properly functioning IL-1Ra, inflammation can build up in your body, causing damage to your connective tissues and organs. These include your skin and bones.
Symptoms of DIRA may include:
- severe skin rash with pustules (raised bumps filled with pus)
- fever
- joint swelling
- bone lesions (areas of damaged bone)
Effectiveness for DIRA
Kineret has been found to be effective in treating DIRA in adults and children, including infants. For details on how the drug performed in clinical trials for DIRA, see Kineret’s prescribing information.
Kineret and children
Kineret is approved to treat NOMID and DIRA in children, including infants. For more information, see the sections just above.
To learn how well Kineret worked for children in clinical trials, see the drug’s prescribing information.
As with all medications, the price of Kineret can vary.
The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
It’s important to note that you’ll have to get Kineret at a specialty pharmacy called Biologics. This type of pharmacy is authorized to carry specialty medications. These are drugs that may be expensive or may require the help of a healthcare professional to be used safely and effectively. For more information, you can call 800-850-4306 or visit the pharmacy’s website.
Before approving coverage for Kineret, your insurance company may require you to get prior authorization. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the prior authorization request and decide if the drug will be covered.
If you’re not sure if you’ll need to get prior authorization for Kineret, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Kineret, or if you need help understanding your insurance coverage, help is available.
Sobi, the manufacturer of Kineret, offers some financial assistance programs. For more information and to find out if you’re eligible for support, call 866-547-0644 or visit the manufacturer’s website.
To learn more about saving money on prescriptions, check out this article.
Biosimilar form
Kineret is available only as a brand-name drug. It’s a biologic medication, which is a drug that’s made from living cells. The active drug in Kineret is anakinra, which is a protein made from E. coli bacteria cells.
Currently, Kineret doesn’t have a biosimilar version. A biosimilar is a medication that’s similar to a brand-name biologic drug. As with generics, biosimilars tend to cost less than brand-name medications.
Here are answers to some frequently asked questions about Kineret.
Is Kineret a biologic?
Yes, Kineret is a biologic drug, also known as a “biologic.” Biologic drugs are made from living cells. The active drug in Kineret is anakinra, which is a protein made from E. coli bacteria cells.
Similar to some other biologics, Kineret has limited distribution. This means the drug is only available from a certain specialty pharmacy. Kineret is distributed by a specialty pharmacy called Biologics. For more information, you can call 800-850-4306 or visit the pharmacy’s website.
Can Kineret be prescribed for pericarditis?
The Food and Drug Administration (FDA) hasn’t approved Kineret for pericarditis. (With pericarditis, you have inflammation [swelling] of the pericardium, a thin, double-layered sac that surrounds your heart.) Doctors may prescribe Kineret off-label for this condition. Off-label drug use is when an FDA-approved drug is prescribed for a purpose other than what it’s approved for.
Small clinical trials have studied whether Kineret may be useful for treating acute (short-term) or recurrent pericarditis. Larger trials are needed to confirm if Kineret is safe and effective for this use.*
Is Kineret an immunosuppressant?
Yes, Kineret is a type of immunosuppressant. Immunosuppressants are drugs that work by reducing the body’s immune response. Typically, the immune response creates inflammation, which can worsen symptoms of many conditions. This includes the conditions that Kineret is prescribed to treat.*
Kineret can weaken your immune system by causing neutropenia as a side effect.† Neutropenia occurs when your body has low levels of neutrophils, a type of white blood cell. (Neutrophils are important for fighting infections.)
During Kineret treatment, it’s important to avoid getting an infection. Try to practice good hand hygiene and avoid coming into contact with people who may be sick.
* To learn more about the FDA-approved uses for Kineret, see “Kineret uses” above. † To learn more about the side effects of Kineret, see the “Kineret side effects” section above.
Alcohol isn’t known to interact with Kineret. However, drinking alcohol may worsen the symptoms of the conditions Kineret is approved to treat.*
Drinking alcohol may also cause some of the same side effects as Kineret. These include nausea, vomiting, or headache. So, drinking alcohol during Kineret treatment may worsen these side effects.†
If you drink alcohol, talk with your doctor about how much, if any, is safe for you to drink during Kineret treatment.
* To learn more about the FDA-approved uses for Kineret, see “Kineret uses” above. † To learn more about the side effects of Kineret, see the “Kineret side effects” section above.
Kineret can interact with certain other medications and certain vaccines.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Kineret and other medications
Below is a list of medications that can interact with Kineret. This list does not contain all drugs that may interact with Kineret.
- Tumor necrosis factor (TNF) blockers, also called TNF-alpha inhibitors, may increase the risk of infection* if used along with Kineret. So, doctors typically will not prescribe Kineret with TNF blockers. Some examples include:
Before taking Kineret, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you take. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
* For more information, see “Side effect details” in the “Kineret side effects” section above.
Kineret and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Kineret. However, you should still check with your doctor or pharmacist before using any of these products during Kineret treatment.
Kineret and foods
There aren’t any foods that have been specifically reported to interact with Kineret. If you have any questions about eating certain foods with Kineret, talk with your doctor.
Kineret and vaccines
You should not receive live vaccines during Kineret treatment. This is because the drug may suppress (weaken) your immune system.
Vaccines are meant to protect you from becoming severely ill from certain diseases. With live vaccines, you receive a small amount of a living pathogen (germ), such as a virus. This helps your immune system recognize and fight that pathogen in the future. However, if your immune system is weakened from Kineret treatment, your body likely won’t be able to respond to the vaccine properly. Instead, you may develop the infection that the vaccine was meant to protect you from.
Before you begin Kineret, your doctor will talk with you about whether you may need any live vaccines. You and your doctor may decide to wait to start Kineret treatment until after you’ve received the live vaccines you need.
Examples of live vaccines you should avoid during Kineret treatment include:
- measles, mumps, rubella
- intranasal influenza (FluMist)
- chickenpox
- rotavirus
- typhoid
- yellow fever
Before you receive any vaccine, check with the healthcare professional giving you the vaccine to make sure it isn’t a live vaccine. And be sure to tell them that you’re taking Kineret, a medication that weakens the immune system.
The Food and Drug Administration (FDA) has approved Kineret to treat rheumatoid arthritis (RA), an autoimmune condition. It’s also approved to treat neonatal-onset multisystem inflammatory disease (NOMID) and deficiency of interleukin-1 receptor antagonist (DIRA). These are rare genetic conditions that start at birth. For more information about these conditions, see the “Kineret uses” section above.
What Kineret does
Kineret is a type of biologic drug called an interleukin-1 receptor antagonist (IL-1Ra). Biologic drugs are made from living cells. IL-1Ra is a protein that your body’s immune system makes naturally. This protein usually works to block the activity of IL-1, a protein in the body that causes inflammation (swelling).
Kineret contains the active ingredient anakinra, which is a recombinant (slightly modified) version of IL-1Ra. The drug acts like the body’s natural IL-1Ra protein. For example, in people with DIRA, the IL-1Ra protein doesn’t work as it should, and Kineret replaces it.
Kineret works by blocking the activity of IL-1. So the drug works to reduce inflammation and related symptoms due to the conditions it’s approved to treat. These include RA, NOMID, and DIRA.
Inflammation occurs as part of your body’s immune response. For example, inflammation happens when your body fights off infection. However, with inflammatory conditions, the immune response is overactive and mistakenly attacks the body’s own tissues. This creates excessive inflammation, which can lead to severe symptoms and tissue damage.
If you have questions about how Kineret works to treat your condition, talk with your doctor or pharmacist.
How long does it take to work?
To treat RA, Kineret may take a while to work. In clinical trials, Kineret improved symptoms within 3 months to 6 months in people with RA. However, not everyone who takes Kineret for RA may have the same results.
For NOMID or DIRA treatment, Kineret typically starts working right away. However, it may take some time for you and your doctor to find the dosage that works best for you. (For more information on dosage, see the “Kineret dosage” section above.)
It isn’t known if Kineret treatment is safe during pregnancy. The medication hasn’t been studied in enough pregnant people to know for sure. Animal studies haven’t shown any risks to developing fetuses when the drug was given during pregnancy. However, animal studies don’t always reflect what happens in humans.
If you become pregnant or think you may be pregnant during Kineret treatment, talk with your doctor.
It’s not known if Kineret is safe to take during pregnancy. If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs during Kineret treatment.
For more information about using Kineret during pregnancy, see the “Kineret and pregnancy” section above.
It’s unknown if Kineret treatment is safe while breastfeeding. The drug’s effects on human breast milk or breastfed children haven’t been studied.
If you’re breastfeeding or planning to breastfeed, talk with your doctor before starting Kineret treatment. They can discuss the benefits and risks of the treatment options for your condition.
This drug comes with several precautions.
Before taking Kineret, talk with your doctor about your health history. Kineret may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Kidney problems. If you have kidney problems, your doctor may prescribe a lower dosage of the drug for you. They may also monitor your kidney health during Kineret treatment. (For more information on dosage, see the “Kineret dosage” section above.)
- Infection. Kineret may weaken your immune system and reduce your body’s ability to fight off infection. If you have any type of infection, your doctor typically won’t have you start Kineret treatment. Tell your doctor about your infection. They’ll likely treat your infection or wait until it’s gone before prescribing Kineret.
- Allergic reaction. If you’ve had an allergic reaction to Kineret or any of its ingredients, your doctor will likely not prescribe Kineret. Ask your doctor what other medications are better options for you.
- Pregnancy. It isn’t known if Kineret treatment is safe during pregnancy. For more information, see the “Kineret and pregnancy” section above.
- Breastfeeding. It’s unknown if Kineret treatment is safe while breastfeeding. For more details, see the “Kineret and breastfeeding” section above.
Note: For more information about the potential negative effects of Kineret, see the “Kineret side effects” section above.
Do not inject more Kineret than your doctor recommends. For some drugs, doing so may lead to unwanted side effects or overdose.
What to do in case you inject too much Kineret
If you think you’ve injected too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. However, if your symptoms are severe, call 911 or your local emergency number, or go to the nearest emergency room right away.
When you get Kineret from the pharmacy, the pharmacist will add an expiration date to the label on the packaging. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee that the medication is effective during this time. The current stance of the Food and Drug Administration (FDA) is to avoid using expired medications. Kineret’s manufacturer advises not using Kineret past the expiration date on the packaging.
Storage
How long a medication remains good to use can depend on many factors, including how and where you store the medication.
Kineret syringes should be stored in the refrigerator at 36°F to 46°F (2°C to 8°C). They should be stored in their original packaging to protect them from light. Discard any syringe that has been out of the refrigerator for more than 12 hours. Do not use them to inject your doses.
Avoid storing this medication in areas where it could get damp or wet, such as bathrooms.
Disposal
Right after you’ve used a syringe, needle, or autoinjector, dispose of it in an FDA-approved sharps disposal container. This helps prevent others, including children and pets, from injecting the drug by accident or harming themselves with the needle. You can buy a sharps container online, or ask your doctor, pharmacist, or health insurance company where to get one.
This article provides several useful tips on medication disposal. You can also ask your pharmacist for information about how to dispose of your medication.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.