Tumor Metastasis: Molecular Insights and Evolving Paradigms (original) (raw)
. Author manuscript; available in PMC: 2012 Oct 14.
Abstract
Metastases represent the end-products of a multi-step cell-biological process termed the invasion-metastasis cascade, which involves dissemination of cancer cells to anatomically distant organ sites and their subsequent adaptation to foreign tissue microenvironments. Each of these events is driven by (1) acquisition of genetic and/or epigenetic alterations within tumor cells and (2) co-option of non-neoplastic stromal cells, which together endow incipient metastatic cells with traits needed to generate macroscopic metastases. Recent advances have provided provocative insights regarding these cell-biological and molecular changes, which carry implications concerning the pathogenesis of metastatic progression and the steps of the invasion-metastasis cascade that appear amenable to therapeutic targeting.
While surgical resection and adjuvant therapy can cure well-confined primary tumors, metastatic disease is largely incurable because of its systemic nature and the resistance of disseminated tumor cells to existing therapeutic agents. This explains why >90% of mortality from cancer is attributable to metastases, not the primary tumors from which these malignant lesions arise (Gupta and Massagué, 2006; Steeg, 2006). As such, our ability to effectively treat cancer is largely dependent on our capacity to interdict – and perhaps even reverse – the process of metastasis.
These clinical realities have been appreciated for decades. Only recently, however, have molecular and cell-biological details of the mechanisms underlying metastasis emerged. We focus here on the tumors arising in epithelial tissues – carcinomas – which together constitute ~80% of life-threatening cancers. We highlight recent discoveries, discuss their conceptual implications, and consider their potential clinical utility. Taken together, these advances have established new paradigms that are likely to guide future research on metastasis, as well as the development of novel diagnostic and therapeutic strategies.
The Invasion-Metastasis Cascade
The metastases spawned by carcinomas are formed following the completion of a complex succession of cell-biological events – collectively termed the invasion-metastasis cascade – whereby epithelial cells in primary tumors (1) invade locally through surrounding extracellular matrix (ECM) and stromal cell layers, (2) intravasate into the lumina of blood vessels, (3) survive the rigors of transport through the vasculature, (4) arrest at distant organ sites, (5) extravasate into the parenchyma of distant tissues, (6) initially survive in these foreign microenvironments in order to form micrometastases, and (7) re-initiate their proliferative programs at metastatic sites, thereby generating macroscopic, clinically detectable neoplastic growths (the step often referred to as “metastatic colonization”) (Figure 1) (Fidler, 2003). As discussed below, many of these complex cell-biological events are orchestrated by molecular pathways operating within carcinoma cells. Importantly, cell-non-autonomous interactions between carcinoma cells and non-neoplastic stromal cells also play vital roles throughout the invasion-metastasis cascade (Figure 2). Deregulation of these intrinsic and extrinsic signaling cascades allows incipient metastatic carcinoma cells to generate high-grade, life-threatening malignancies.
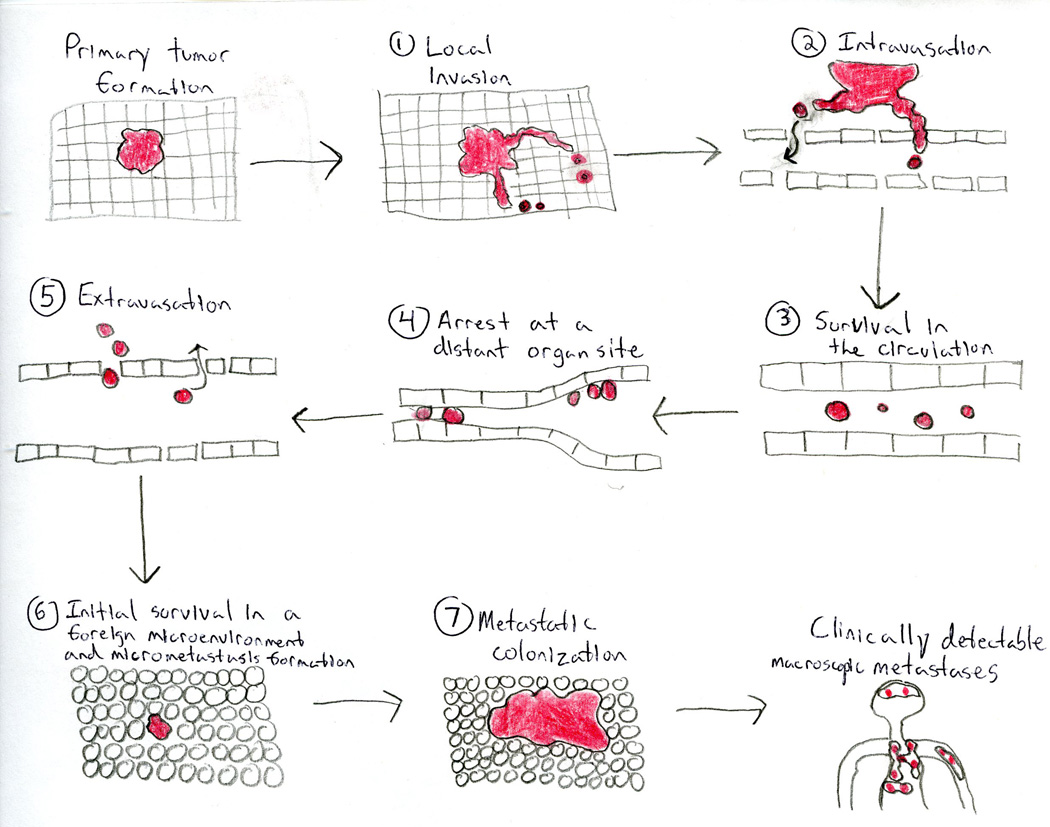
Figure 1. The Invasion-Metastasis Cascade.
Clinically detectable metastases represent the end-products of a complex series of cell-biological events, which are collectively termed the invasion-metastasis cascade. During metastatic progression, tumor cells exit their primary sites of growth (local invasion, intravasation), translocate systemically (survival in the circulation, arrest at a distant organ site, extravasation), and adapt to survive and thrive in the foreign microenvironments of distant tissues (initial survival in a foreign microenvironment and micrometastasis formation, metastatic colonization). Carcinoma cells are depicted in red.
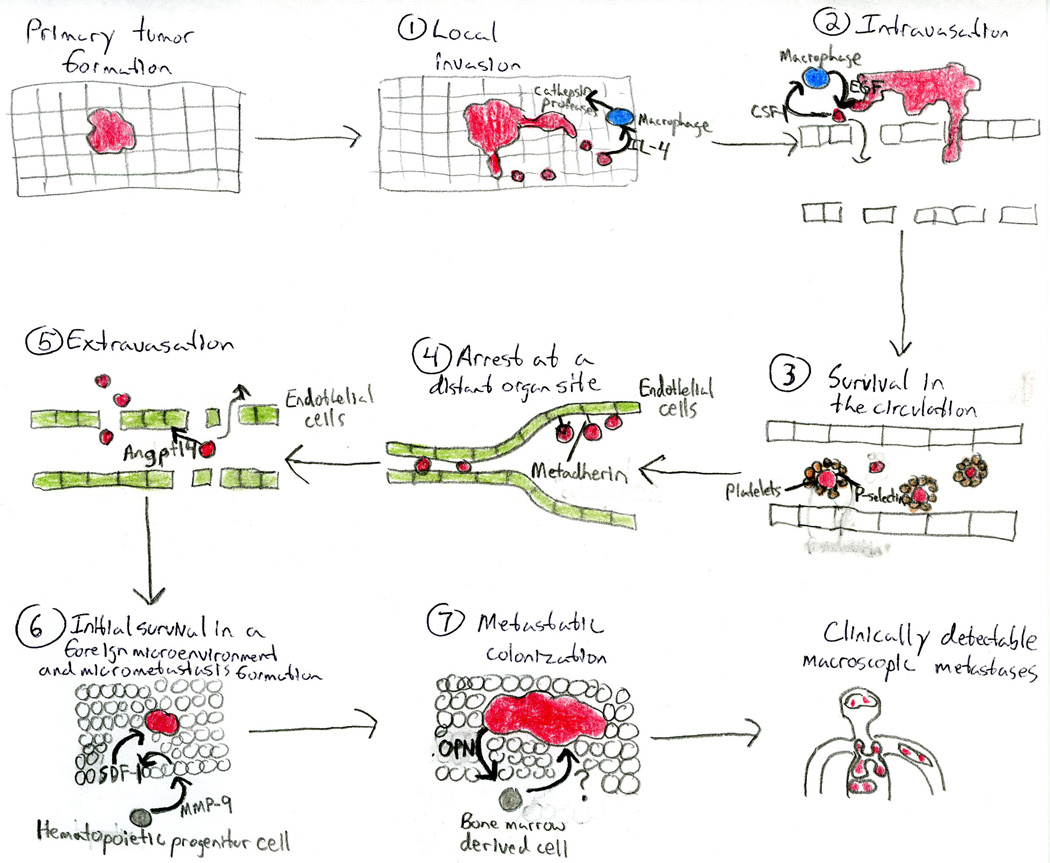
Figure 2. Stromal Cells Play Imperative Roles During Every Step of the Invasion-Metastasis Cascade.
Metastatic progression is not an exclusively cell-autonomous process. Indeed, carcinoma cells enlist non-neoplastic stromal cells to aid in each step of the invasion-metastasis cascade. Examples of the roles of stromal cells during metastasis are illustrated. Carcinoma cells are depicted in red. Angptl4: angiopoietin-like-4; CSF-1: colony stimulating factor-1; EGF: epidermal growth factor; IL-4: interleukin-4; MMP-9: matrix metalloproteinase- 9; OPN: osteopontin; SDF-1: stromal cell-derived factor-1.
1. Local Invasion
Local invasiveness involves entry of cancer cells that have resided within a well-confined primary tumor into the surrounding tumor-associated stroma and thereafter into the adjacent normal tissue parenchyma. In order to invade the stroma, carcinoma cells must first breach the basement membrane (BM) – a specialized ECM that plays vital roles in organizing epithelial tissues, in part by separating their epithelial and stromal compartments. In addition to structural roles played by the BM, components of this ECM contain a repository of tethered growth factor molecules that can be liberated by carcinoma-secreted proteases. Moreover, the BM also plays crucial roles in signal transduction events within carcinoma cells via pathways initiated by integrin-mediated cell-matrix adhesions, leading to alterations in cell polarity, proliferation, invasiveness, and survival (Bissell and Hines, 2011).
Emerging evidence indicates that the precisely controlled tissue architecture of normal epithelium serves as an intrinsic barrier to invasiveness that must be overcome by incipient metastatic carcinoma cells before they can develop into overt malignancies. For example, in the mammary gland, myoepithelial cells oppose invasion by helping to maintain BM integrity; indeed, co-implantation with myoepithelial cells reversed the invasiveness of breast carcinoma xenografts (Hu et al., 2008). Similarly, in ovarian carcinomas, the mesothelial cell layer that lines peritoneal and pleural organs serves as an obstacle to further dissemination that can be overcome by carcinoma cell-exerted, myosin-dependent traction forces that physically displace mesothelial cells (Iwanicki et al., 2011). Moreover, modulation of ECM stiffness, achieved by altering collagen crosslinking, affects breast carcinoma progression via altered integrin signaling (Levental et al., 2009).
At a cell-biological level, most types of carcinomas can invade as cohesive multi-cellular units through a process termed “collective invasion”. Alternatively, individual tumor cells may invade via two distinct programs: the protease-, stress-fiber-, and integrin-dependent “mesenchymal invasion” program or the protease-, stress-fiber-, and integrin-independent, Rho/ROCK-dependent “amoeboid invasion” program (Friedl and Wolf, 2003). Indeed, differential expression of molecules that enable either mesenchymal or amoeboid invasion can be observed in signatures of local invasiveness derived from mammary carcinoma models (Wang et al., 2004).
Tumor cells can apparently interconvert between these various invasion strategies in response to changing microenvironmental conditions. This has caused some to propose that robust suppression of single-cell invasion requires concomitant inhibition of the mesenchymal and amoeboid invasion programs (Friedl and Wolf, 2003). Indeed, certain regulators of invasion function as pleiotropically acting factors that simultaneously modulate components of both pathways. For example, the microRNA (miRNA) miR-31 inhibits breast cancer invasion via concurrent suppression of key effectors of both the mesenchymal (e.g., integrin α5) and amoeboid (e.g., RhoA) invasion programs (Valastyan et al., 2009).
The single-cell invasion pathways cited above are clearly incompatible with one critical element of epithelial tissue organization, specifically the E-cadherin-mediated intercellular junctions that knit together epithelial cell sheets and prevent dissociation of individual epithelial cells from their neighbors. In order to overcome this and other obstacles to invasion, carcinoma cells may co-opt a cell-biological program known as epithelial-mesenchymal transition (EMT), which is critical for multiple aspects of normal embryonic morphogenesis. The EMT program – which involves dissolution of adherens and tight junctions and a loss of cell polarity – dissociates the cells within epithelial cell sheets into individual cells that exhibit multiple mesenchymal attributes, including heightened invasiveness (Thiery et al., 2009).
EMT programs are orchestrated by a set of pleiotropically acting transcription factors (TFs) – including Slug, Snail, Twist, ZEB1, and ZEB2 – which organize entrance into a mesenchymal state by suppressing expression of epithelial markers and inducing expression of other markers associated with the mesenchymal state (Thiery et al., 2009). Indeed, several of these TFs directly repress levels of E-cadherin, the keystone of the epithelial state. Certain miRNAs – notably those belonging to the miR-200 family – also regulate EMT programs. One important mechanism by which miR-200 promotes an epithelial phenotype involves its ability to post-transcriptionally suppress expression of the ZEB1 and ZEB2 EMT-inducing TFs. Acting in the opposite direction, ZEB1 and ZEB2 transcriptionally repress miR-200 family members, thereby establishing a double-negative-feedback loop that operates as a bi-stable switch, reinforcing the residence of cells in either the mesenchymal or epithelial state (Thiery et al., 2009).
Ultimately, loss of the BM barrier allows direct invasion by carcinoma cells of the stromal compartment. Active proteolysis, effected principally by matrix metalloproteinases (MMPs), drives this loss. In normal tissue, the activity of MMPs is carefully controlled via transcriptional and post-translational mechanisms. Carcinoma cells have devised numerous means by which to derail the normally tight control of MMP activity, almost invariably leading to enhanced MMP function. While degrading the BM and other ECM that lies in the path of invading tumor cells, MMP-expressing cells also liberate growth factors that are sequestered there, thereby fostering cancer cell proliferation (Kessenbrock et al., 2010).
Once invading carcinoma cells have dissolved the BM, they enter the stroma. Here they are confronted with a variety of tumor-associated stromal cells, whose composition is governed by the state of tumor progression. As primary tumor progression proceeds, the stroma becomes increasingly “reactive” and acquires many of the attributes of the stroma of tissues that are in the midst of wound healing or are chronically inflamed (Grivennikov et al., 2010). Accordingly, tumor cells invading into a reactive stroma encounter fibroblasts and myofibroblasts, endothelial cells, adipocytes, and various bone marrow-derived cells – including mesenchymal stem cells, as well as macrophages and other immune cells (Joyce and Pollard, 2009).
These stromal cells are capable of further enhancing the aggressive behaviors of carcinoma cells through various types of heterotypic signaling. For example, breast cancer invasiveness can be stimulated through the secretion of interleukin-6 (IL-6) by adipocytes present in the local microenvironment (Dirat et al., 2011). Furthermore, stromal CD4+ T-lymphocytes promote mammary carcinoma invasion by stimulating tumor-associated macrophages (TAMs) to activate epidermal growth factor receptor (EGFR) signaling in the carcinoma cells (DeNardo et al., 2009). Similarly, secretion of IL-4 by breast cancer cells triggers cathepsin protease activity in TAMs, further augmenting carcinoma cell invasiveness (Gocheva et al., 2010). These findings provide examples of the bi-directional interactions that occur between tumor cells and the nearby stroma: carcinoma cells stimulate the formation of an inflamed stroma, and the latter reciprocates by enhancing the malignant traits of the carcinoma cells, thereby established a potentially self-amplifying positive-feedback loop.
Detailed characterizations of stromal cells provide further evidence of their critical roles in enabling the malignant behavior of carcinoma cells. For example, microarray profiling of the tumor-associated stroma derived from breast cancer patients reveals characteristic expression signatures associated with metastatic outcome (Finak et al., 2008). Additionally, an expression signature that typifies the transcriptional response of cultured fibroblasts to serum – and thus reflects one component of wound-healing responses – correlates with increased risk of metastatic recurrence in human breast, gastric, and lung carcinomas (Chang et al., 2004). Such observations are consistent with the role of an increasingly activated stroma in driving malignant behavior in closely apposed carcinoma cells, but they hardly prove causality. Instead, such evidence has begun to emerge from experimental models. For example, perturbation of Hedgehog signaling or caveolin-1 specifically within the stroma alters tumor progression in neighboring carcinoma cells (Olive et al., 2009; Goetz et al., 2011).
Independent of the detailed mechanisms of stromal-epithelial interactions within primary carcinomas, it is clear that entry of neoplastic cells into the stroma provides abundant opportunities for tumor cells to directly access the systemic circulation and thereby disseminate to distant sites.
2. Intravasation
Intravasation involves locally invasive carcinoma cells entering into the lumina of lymphatic or blood vessels. While lymphatic spread of carcinoma cells is routinely observed in human tumors – and represents an important prognostic marker for disease progression – dissemination via the hematogenous circulation appears to represent the major mechanism by which metastatic carcinoma cells disperse (Gupta and Massagué, 2006).
Intravasation can be facilitated by molecular changes that promote the ability of carcinoma cells to cross the pericyte and endothelial cell barriers that form the walls of microvessels. For example, the transcriptional modulator amino-terminal enhancer of split (Aes) inhibited the intravasation of colon carcinoma cells by impairing trans-endothelial invasion through Notch-dependent mechanisms (Sonoshita et al., 2011). Conversely, the cytokine transforming growth factor-β (TGFβ) enhanced mammary carcinoma intravasation, ostensibly by increasing carcinoma cell penetration of microvessel walls or augmenting invasiveness more generally (Giampieri et al., 2009). Additionally, the intravasation of breast carcinoma cells can be enhanced by perivascular TAMs via a positive-feedback loop comprised of the reciprocal secretion of epidermal growth factor (EGF) and colony stimulating factor-1 (CSF-1) by TAMs and carcinoma cells, respectively (Wyckoff et al., 2007).
The mechanics of intravasation are likely to be strongly influenced by the structural features of tumor-associated blood vessels. Through a variety of mechanisms – many of which converge on the actions of vascular endothelial growth factors (VEGFs) – tumor cells stimulate the formation of new blood vessels within their local microenvironment via the process termed neoangiogenesis. In contrast to blood vessels present in normal tissues, the neovasculature generated by carcinoma cells is tortuous, prone to leakiness, and in a state of continuous reconfiguration (Carmeliet and Jain, 2011). The weak interactions between adjacent endothelial cells that form the tumor-associated microvasculature and the absence of extensive pericyte coverage are likely to facilitate intravasation. In support of this notion, the capacity of cyclooxygenase-2 (COX-2), epiregulin (EREG), MMP-1, and MMP-2 to synergistically promote breast carcinoma intravasation was tied to their ability to stimulate neoangiogenesis and the formation of leaky blood vessels (Gupta et al., 2007a).
3. Survival in the Circulation
Once carcinoma cells have successfully intravasated into the lumina of blood vessels, they can disseminate widely through the venous and arterial circulation. Recent technological advances have facilitated detection of circulating tumor cells (CTCs) within the bloodstream of carcinoma patients (Nagrath et al., 2007; Pantel et al., 2008; Stott et al., 2010). CTCs ostensibly represent carcinoma cells that are en route between primary tumors and sites of dissemination and therefore may represent “metastatic intermediates”.
CTCs in the hematogenous circulation must survive a variety of stresses in order to reach distant organ sites. For example, they would seem to be deprived of the integrin-dependent adhesion to ECM components that is normally essential for cell survival. In the absence of such anchorage, epithelial cells normally undergo anoikis – a form of apoptosis triggered by loss of anchorage to substratum (Guo and Giancotti, 2004). Some of the signaling events that oversee anoikis responses impinge upon metabolic programs, such as the pentose phosphate pathway and control of glucose uptake (Schafer et al., 2009). Also of interest, the tyrosine kinase TrkB was identified as a suppressor of anoikis whose expression was required for metastatic progression in transformed intestinal epithelial cells (Douma et al., 2004).
A more nuanced understanding of the lives of CTCs is precluded at present by the dearth of simple facts: we do not know how long cancer cells linger in the circulation. Some have estimated that their dwell time in breast cancer patients may be several hours (Meng et al., 2004). However, given the relatively large diameters of carcinoma cells (20–30 µm) and the luminal diameter of capillaries (~8 µm), the vast majority of CTCs are likely to become trapped in various capillary beds during their first passes through the circulation (i.e., within minutes of intravasation). It is therefore possible that many tumor cells spend only relatively brief periods of time in the bloodstream, allowing CTCs to escape from the circulation long before anoikis alarms are sounded.
In addition to stresses imposed by matrix detachment, tumor cells in the circulation must overcome the damage incurred by hemodynamic shear forces and predation by cells of the innate immune system – specifically natural killer cells. Conveniently, carcinoma cells seem to simultaneously evade both of these threats through a single mechanism that depends on co-opting one aspect of normal blood coagulation. More specifically, by forming relatively large emboli via interactions with blood platelets – a process that appears to be mediated by the expression of Tissue Factor and/or L- and P-selectins by the carcinoma cells – tumor cells are able to both shield themselves from shear forces and evade immune detection (Joyce and Pollard, 2009). Thus, platelet-coated tumor cells are better able to persist within the circulation until they arrest at distant tissue sites, an event whose likelihood may be further increased due to the large effective diameter of these microemboli.
4. Arrest at a Distant Organ Site
Despite the theoretical ability of hematogenously traveling CTCs to disseminate to a wide variety of secondary loci, clinicians have long noted that individual carcinoma types form metastases in only a limited subset of target organs (Figure 3) (Fidler, 2003). A major unresolved issue concerns whether this tissue tropism simply reflects a passive process whereby CTCs arrest within capillary beds due to the layout of the vasculature and size restrictions imposed by blood vessel diameters or, instead, indicates a capacity of CTCs to actively home to specific organs via genetically templated ligand-receptor interactions between these cells and the luminal walls of the microvasculature.
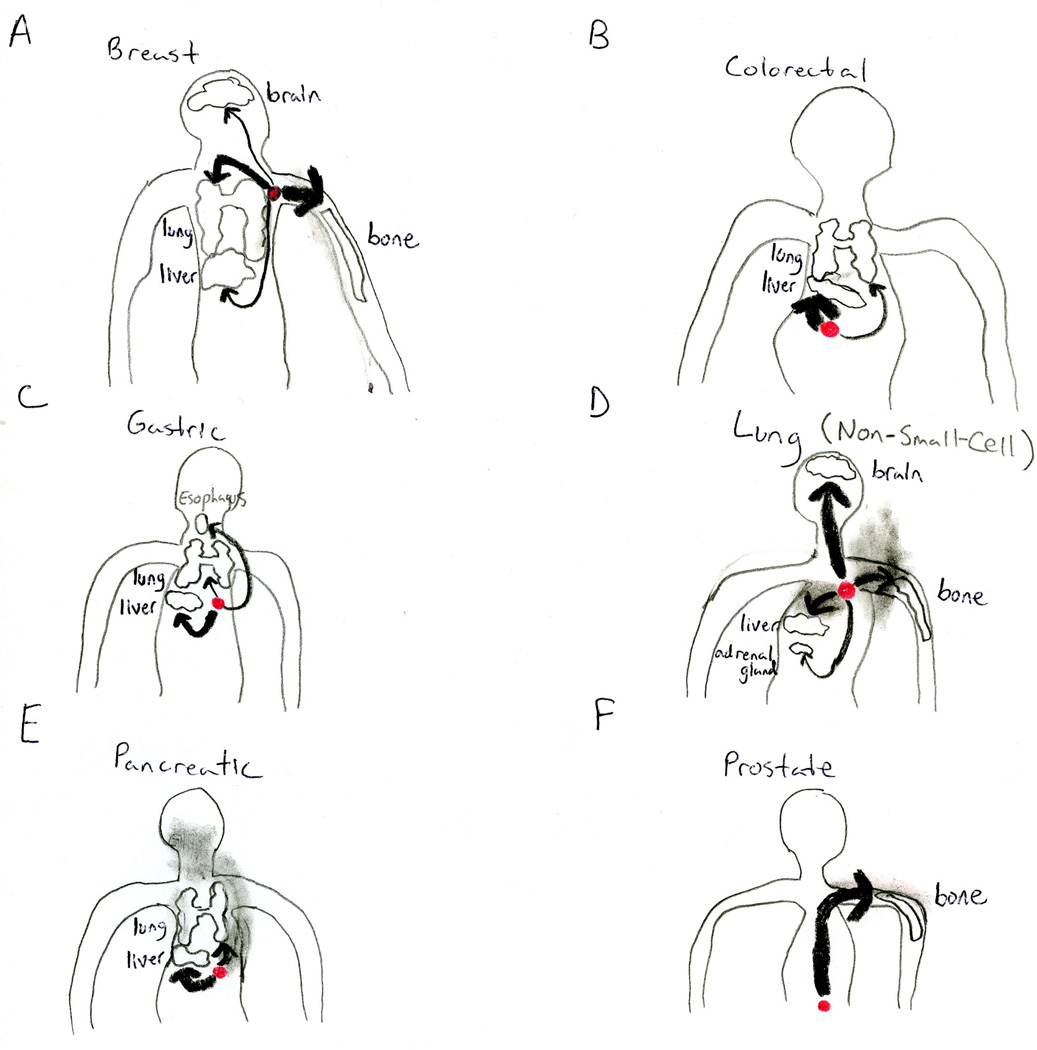
Figure 3. Metastatic Tropism.
Carcinomas originating from a particular epithelial tissue form detectable metastases in only a limited subset of theoretically possible distant organ sites. Shown here are the most common sites of metastasis for six well-studied carcinoma types. Primary tumors are depicted in red. Thickness of black lines reflects the relative frequencies with which a given primary tumor type metastasizes to the indicated distant organ site.
The issue of physical trapping of CTCs in microvessels looms large here. For example, the anatomical layout of the vasculature precludes arrest of carcinoma cells within the capillary beds of certain distant organs when those capillary beds lie downstream of other microvessels whose diameter is insufficient to permit passage of CTCs. Most frequently cited is the large-scale trapping of colorectal carcinoma cells in the liver, which is dictated by the portal vein that drains the mesenteric circulation directly into the liver (Gupta and Massagué, 2006). Nevertheless, some CTCs may elude this rapid trapping because of their unusual plasticity or chance passage through arteriovenous shunts, thereby enabling them to become lodged in the microvessels of more distal organs.
The alternative hypothesis is that CTCs have predetermined predilections to lodge in certain tissues. Indeed, some carcinoma cells are capable of forming specific adhesive interactions in particular tissues that preferentially favor their trapping. For example, some have proposed that Metadherin expression in breast cancer cells causes homing to the lungs by facilitating binding to the pulmonary vasculature (Brown and Ruoslahti, 2004). Similarly, entry of colorectal and lung carcinoma cells into the hepatic microvasculature can initiate a pro-inflammatory cascade that results in Kupffer cells being triggered to secrete chemokines that upregulate various vascular adhesion receptors, thereby enabling adhesion of CTCs in the microvasculature of the liver (Auguste et al., 2007). The relative importance of these and other molecularly driven strategies that serve to facilitate the organ-specific arrest of CTCs awaits future study.
5. Extravasation
Once lodged in the microvasculature of distant organs, CTCs may initiate intraluminal growth and form a microcolony that eventually ruptures the walls of surrounding vessels, thereby placing tumor cells in direct contact with the tissue parenchyma (Al-Mehdi et al., 2000). Alternatively, carcinoma cells may cross from vessel lumina into the tissue parenchyma by penetrating the endothelial cell and pericyte layers that separate vessel lumina from the stromal microenvironment – a process known as extravasation.
This latter form of extravasation would seem to represent, at least superficially, the reverse of the earlier step of intravasation. However, there are reasons to believe that these processes may, in fact, oftentimes be quite different mechanistically. While intravasation can be fostered by certain co-opted cell types present in the primary tumor stroma, such as the TAMs described earlier (Wyckoff et al., 2007), these same supporting cells are unlikely to be equally available to facilitate the extravasation of disseminated carcinoma cells. Indeed, macrophage populations that reside in primary tumors are phenotypically and functionally distinct from those present at sites of metastasis formation (Qian and Pollard, 2010). In addition, as discussed previously, the neovasculature formed by primary tumors is tortuous and leaky (Carmeliet and Jain, 2011), while microvessels in distant normal tissues – the destination sites of disseminated cancer cells – are likely to be highly functional, which can result in low intrinsic permeability. For example, disseminated carcinoma cells attempting to reach the brain parenchyma must traverse the blood-brain barrier; similarly, endothelial cells lining pulmonary microvessels normally create a largely impermeable barrier. In contrast, carcinoma cells arriving in the bone or liver encounter fenestrated sinusoids that are highly permeable even in their normal state and consequently would seem to pose only minor obstacles to extravasating tumor cells (Nguyen et al., 2009). Hence, the characteristics of specific microenvironments present at metastatic sites may strongly influence the fate of disseminated carcinoma cells – a critically important point that will be revisited below.
In order to overcome physical barriers to extravasation that operate in tissues with low intrinsic microvessel permeability, primary tumors are capable of secreting factors that perturb these distant microenvironments and induce vascular hyper-permeability. For example, the secreted protein angiopoietin-like-4 (Angptl4) – as well as the pleiotropically acting factors EREG, COX-2, MMP-1, and MMP-2 – disrupt pulmonary vascular endothelial cell-cell junctions in order to foster the extravasation of breast carcinoma cells in the lungs (Gupta et al., 2007a; Padua et al., 2008). Also of interest, angiopoietin2 (Angpt2), MMP-3, MMP-10, placental growth factor, and VEGF secreted by various types of primary tumors are capable of inducing pulmonary hyper-permeability prior to the arrival of carcinoma cells in the lungs, thereby facilitating the subsequent extravasation of CTCs (Weis et al., 2004; Huang et al., 2009; Hiratsuka et al., 2011b). Finally, inflammatory monocytes recruited to pulmonary metastases via CCL2-dependent mechanisms promote the extravasation of breast carcinoma cells in the lungs by secreting VEGF (Qian et al., 2011).
Of special interest, while Anglptl4 enhanced the extravasation of breast carcinoma cells in the lungs, it failed to augment extravasation of these same breast cancer cells in the bone or their intravasation efficiency (Padua et al., 2008). Hence, Anglptl4 specifically promoted the process of extravasation and did so only within the pulmonary tissue microenvironment. These findings provide evidence for a model in which extravasation at certain distant organ sites necessitates cell-biological programs that are not required either for intravasation or for extravasation at alternative sites of dissemination, again highlighting the critical role of the specific tissue microenvironments present at possible sites of metastasis formation.
6. Initial Survival in a Foreign Microenvironment and Micrometastasis Formation
In order to form metastases, extravasated carcinoma cells must survive in the foreign microenvironment that they encounter in the parenchyma of distant tissues. The microenvironment at the metastatic locus usually differs greatly from that present in the site of primary tumor formation. This dictates that disseminated cancer cells are, at least initially, poorly adapted to their new-found homes. These microenvironmental differences may include the types of stromal cells, ECM constituents, available growth factors and cytokines, and even the microarchitecture of the tissue itself.
Some have proposed that carcinoma cells can address the problem of an incompatible microenvironment at the metastatic site via the establishment of a “pre-metastatic niche” (Psaila and Lyden, 2009). According to this model, primary tumors release systemic signals – perhaps including lysyl oxidase (LOX) (Erler et al., 2009) – that induce organ-specific upregulation of fibronectin from resident tissue fibroblasts. This leads, in turn, to mobilization of VEGF-receptor-1-positive (VEGFR1+) hematopoietic progenitor cells from the bone marrow to these future sites of metastasis via homing interactions between the deposited fibronectin and its cognate receptor, integrin α4β1, which is expressed by the hematopoietic progenitor cells. These hematopoietic progenitor cells then modify the local microenvironments at these loci by secreting MMP-9. Activation of MMP-9 at future sites of metastasis is believed to result in stimulation of various integrins, as well as liberation of molecules that have been sequestered in the ECM, such as the carcinoma cell chemoattractant stromal cell-derived factor-1 (SDF-1) (Psaila and Lyden, 2009). Importantly, all of these events are thought to occur prior to the arrival of carcinoma cells at the metastatic loci. Accordingly, these predisposing changes convert distant microenvironments into more hospitable sites for future settling by disseminated tumor cells.
Importantly, the formation of a supportive pre-metastatic niche could represent a broadly important determinant of both metastatic propensity and tissue tropism, as the spectrum of organ-specific metastases generated by disseminating lung carcinoma cells can be altered simply by rerouting the niche-forming hematopoietic cells to different organs (Psaila and Lyden, 2009). We note that certain molecular details underlying the pre-metastatic niche concept have been questioned (Dawson et al., 2009). More generally, however, it is clear that tumor cells deploy complex mechanisms to modify foreign microenvironments in order to initially survive at these ectopic locations and form small micrometastases.
At the same time, disseminated cancer cells must utilize cell-autonomous programs in order to adapt to the demands imposed by foreign tissues. One example of such a mechanism involves activation of Src tyrosine kinase signaling. Depletion of Src activity impaired the capacity of breast carcinoma cells to persist in bone without influencing their initial homing to this tissue. These effects were attributed to Src-dependent modulation of the responsiveness of these carcinoma cells to stroma-derived SDF-1 and TNF-related apoptosis-inducing ligand (TRAIL). Of additional interest, the same Src signaling failed to enhance the ability of breast carcinoma cells to persist in the lung, again underscoring the organ-specific nature of the latter steps of the invasion-metastasis cascade (Zhang et al., 2009).
7. Metastatic Colonization
In the event that disseminated carcinoma cells survive their initial encounter with the microenvironment of a foreign tissue and succeed in persisting, they still are not guaranteed to proliferate and form large macroscopic metastases – the process of metastatic colonization. Instead, it seems that the vast majority of disseminated tumor cells suffer either slow attrition over periods of weeks and months or persist as microcolonies in a state of apparent long-term dormancy, retaining viability in the absence of any net gain or loss in overall cell number (Chambers et al., 2002).
In fact, these occult micrometastases may persist in one of two ways. The disseminated tumor cells may be largely quiescent, with their proliferation at metastatic sites greatly impaired due to incompatibilities with the foreign microenvironments that surround them (Chambers et al., 2002). In mammary carcinoma cells, this quiescence has been attributed to an inability to engage the focal adhesion kinase (FAK), integrin β1, and Src pathways within distant tissues (Barkan et al., 2008; Shibue and Weinberg, 2009; Barkan et al., 2010). Moreover, the ability of disseminated tumor cells to escape dormancy and to begin active proliferation may depend on cell-non-autonomous mechanisms that are needed to convert foreign microenvironments into more hospitable niches. For example, the outgrowth of otherwise-indolent disseminated tumor cells may depend on the activation and mobilization into the circulation of bone marrow-derived cells and the sequent recruitment of these cells to a metastatic site; in some cases, these processes may be stimulated by systemic signals released by carcinoma cells, such as osteopontin (OPN) or SDF-1 (McAllister et al., 2008; Hiratsuka et al., 2011a).
Alternatively, the cancer cells in occult micrometastases may proliferate continuously; however, a net increase in their overall number may not occur due to the counterbalancing effects of a high apoptotic rate. The mechanisms underlying such high rates of attrition remain poorly understood, but a failure of the disseminated tumor cells to trigger neoangiogenesis has been proposed as one explanation for this phenomenon (Chambers et al., 2002). Consistent with this notion, prostate tumor cell-secreted prosaposin (Psap) may inhibit metastatic colonization by inducing expression of the anti-angiogenic factor thrombospondin-1 in stromal cells (Kang et al., 2009). Conversely, Angpt2 appears to facilitate the metastatic colonization of mammary and pancreatic carcinomas by promoting the capacity of infiltrating myeloid cells to support the vascularization of metastatic nodules (Mazzieri et al., 2011).
The appreciation that disseminated tumor cells often encounter significant obstacles as they attempt to reactivate their growth machinery at metastatic sites is hardly a new concept. More than 120 years ago, Stephen Paget articulated his “seed-and-soil” hypothesis of metastatic outgrowth. From autopsy records, Paget observed preferential metastasis of a given type of cancer to one or more particular distant organ sites, which led him to posit that while tumor cells are broadly disseminated during the course of malignant progression, detectable metastases only develop at those sites (“soils”) where the tumor cells (“seeds”) are suitably adapted for survival and proliferation (Fidler, 2003). Stated differently, the anatomical layout of the vasculature is not sufficient to account for the clinically observed patterns of overt metastasis formation; instead, these patterns of metastatic outgrowth must also reflect the adaptability of tumor cells to particular foreign microenvironments.
Consistent with the seed-and-soil hypothesis, evidence from a number of laboratories has documented that specific organ microenvironments are indeed intrinsically more or less hospitable for the proliferation and survival of certain types of disseminated tumor cells. For example, melanoma cells readily metastasized to sub-cutaneous grafts of lung tissue but failed to metastasize to identically placed – and comparably vascularized – sub-cutaneous grafts of renal tissue, thereby recapitulating the known proclivity of melanomas to form pulmonary metastases (Hart and Fidler, 1980).
More recently, a number of genes whose expression facilitates the metastatic colonization of breast cancer cells specifically to either bone (Kang et al., 2003), lung (Minn et al., 2005), brain (Bos et al., 2009), or liver (Tabariès et al., 2011) have been identified. These genes seem to dictate organ-specific metastatic tropism due to their ability to compensate for and overcome incompatibilities between the intrinsic growth programs of the disseminated carcinoma cells and the demands imposed by the particular foreign tissue microenvironment around them.
One striking example of this is provided by the osteoclastic cytokine IL-11, which facilitates the formation of osteolytic bone metastases by breast cancer cells. IL-11 acts via mechanisms that involve perturbing the normal physiologic signaling between osteoblasts and osteoclasts mediated by receptor activator for nuclear factor κB (RANK) (Kang et al., 2003). Analogously, in breast cancer cells, the Notch ligand Jagged1 promotes the formation of osteolytic bone metastases by enhancing osteoclast activity through a mechanism involving osteoblast-secreted IL-6 (Sethi et al., 2011). By favoring osteoclast function, IL-11 and Jagged1 can drive osteolysis and the release of rich deposits of growth factors that are normally sequestered in the bone matrix. Conversely, IL-11 and Jagged1 are expected to offer little benefit to breast carcinoma cells that have landed in the lungs or brain, where osteoclasts do not operate. More generally, this notion that distinct tissue microenvironments impose dramatically different organ-specific requirements for metastatic colonization is illustrated by the minimal overlap between genes identified as candidate mediators of the metastatic colonization of breast cancer cells in bone, lung, brain, or liver (Kang et al., 2003; Minn et al., 2005; Bos et al., 2009; Tabariès et al., 2011).
These findings hold important implications for our understanding of the molecular mechanisms underlying this final step of the invasion-metastasis cascade, since they imply that the distinct adaptive programs governing metastatic colonization may number in the dozens – with each determined by both the (1) tissue-of-origin of the disseminating primary tumor cells and (2) identity of the organ site at which metastatic colonization occurs. Stated differently, it is known, for example, that (1) breast carcinoma cells colonizing the bone utilize different molecular programs than do prostate carcinoma cells colonizing the same bone tissue and (2) breast carcinoma cells colonizing the lungs utilize different genetic and/or epigenetic programs than do the same breast carcinoma cells colonizing the bone, brain, or liver (Figure 4).
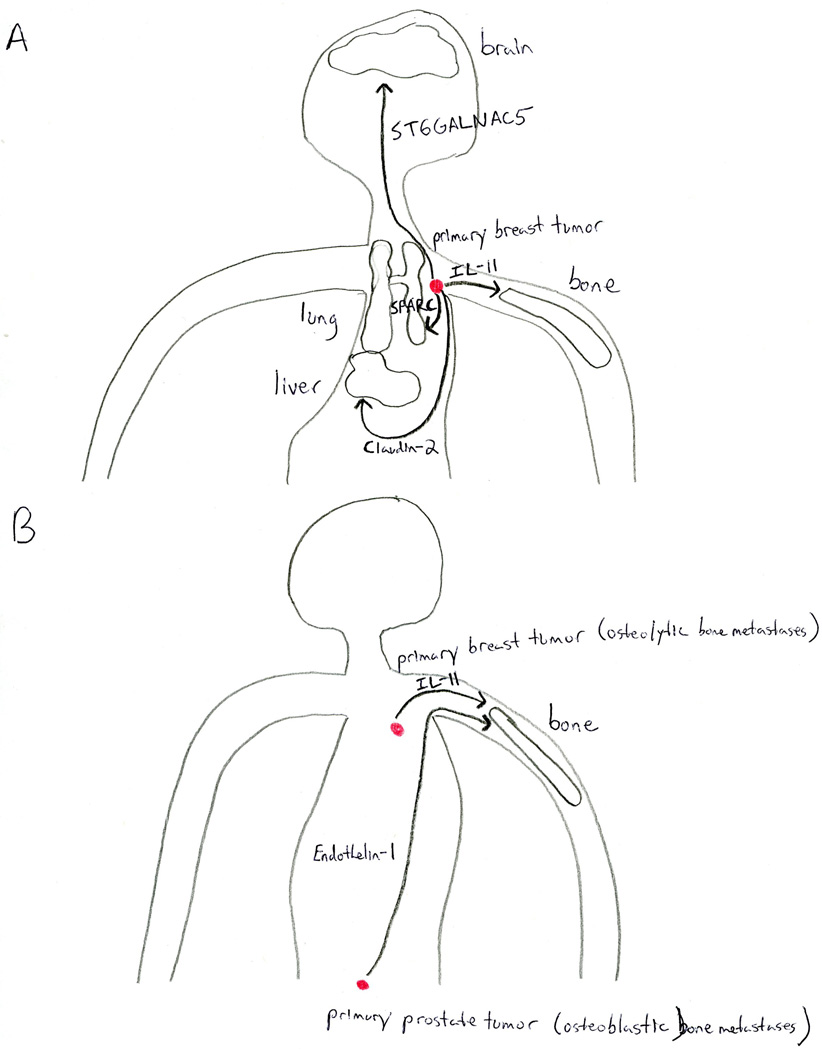
Figure 4. Organ-Site- and Primary-Tumor-Type-Specificity of Metastatic Colonization.
The number of distinct molecular programs required for metastatic colonization is incredibly high, due to considerations stemming from both the distant organ site that is being colonized and the tissue-of-origin of the primary tumor from which the metastases were initially spawned. (A) An individual primary tumor deploys distinct genetic and/or epigenetic programs in order to colonize different metastatic sites. Accordingly, a primary breast tumor (depicted in red), utilizes unique signal transduction pathways to metastasize to bone, brain, liver, or lung. (B) Carcinomas originating from two different tissues may deploy distinct molecular programs in order to colonize the same metastatic organ site. For example, primary breast tumors (upper red lesion) initiate signaling pathways that yield osteolytic bone metastases, while primary prostate tumors (lower red lesion) spawn osteoblastic bone metastases that are driven by unrelated molecular programs. IL-11: interleukin-11; SPARC: secreted protein acidic and rich in cysteine; ST6GALNAC5: ST6 (alpha-N-acetyl-neuraminyl-2,3-beta-galactosyl-1,3)-Nacetylgalactosaminide alpha-2,6-sialyltransferase-5.
Success in metastatic colonization is also likely to be influenced by another attribute of the founding cells: they must possess a high self-renewal capacity in order to spawn large malignant growths. Some have proposed that only a subpopulation of the neoplastic cells present within a tumor – the so-called “tumor-initiating cells” (TICs) – possess such an extensive self-renewal capacity. Indeed, xenograft serial transplantation studies involving several tumor types lend support to this model, although the applicability of these findings to all types of human malignancies continues to be debated (Shackleton et al., 2009; Clevers, 2011). Of particular relevance to metastatic colonization, the TIC hypothesis asserts that one or more self-renewing TICs must disseminate during the course of disease progression in order for macroscopic metastases to develop; conversely, the limited self-renewal capacity of disseminated non-TICs may preclude them from spawning macroscopic metastases.
One class of molecules that promote entrance into the TIC-state are EMT-promoting TFs, such as Snail, Twist, and ZEB1. As discussed above, these TFs were initially characterized in the context of cancer for their powers to enhance local invasion. Subsequently, however, EMT-inducing TFs were also discovered to confer self-renewal properties upon carcinoma cells (Thiery et al., 2009). This unexpected convergence between a molecular pathway that promotes both invasiveness and self-renewal is noteworthy, as these TFs appear to concomitantly facilitate physical dissemination of carcinoma cells and – following dissemination – the proliferation of these cells at distant organ sites. Similarly, several miRNAs involved in regulating the EMT also exert control over the TIC-state, including those of the miR-200 family (Shimono et al., 2009).
In addition to components of the EMT regulatory circuitry, the TFs that are members of the inhibitor of cell differentiation (ID) TF family – namely, ID1 and ID3 – and the homeobox TF Nkx2-1 appear to regulate metastatic colonization in carcinomas of the breast and lung, respectively, due to their capacity to modulate the TIC-state (Gupta et al., 2007b; Winslow et al., 2011). Of additional interest, the luminal cell differentiation-promoting TF GATA-3 suppresses mammary carcinoma metastasis through pathways that appear to impinge upon TIC biology (Kouros-Mehr et al., 2008). Finally, the ECM protein tenascin C is capable of stimulating metastatic colonization of the lung by breast cancer cells via perturbation of the Notch and Wnt signal transduction cascades – two circuitries that have previously been linked to the TIC phenotype (Oskarsson et al., 2011).
By concurrently solving microenvironmental incompatibilities and activating self-renewal pathways, a small minority of disseminated carcinoma cells may succeed in completing the process of metastatic colonization and thereby generate macroscopic, clinically detectable metastases. The formation of robustly growing macroscopic metastases represents the endpoint of the invasion-metastasis cascade. In many respects, only those foci that have completed metastatic colonization should be referred to as “metastases”, as these are the only malignant growths that have overcome the daunting series of obstacles that normally operate to oppose metastasis formation.
Of note, many identified regulators of metastasis function pleiotropically to orchestrate multiple steps of the invasion-metastasis cascade. One example of this is supplied by the miRNA miR-31, which suppresses breast cancer metastasis by concurrently impinging upon at least three distinct steps of the invasion-metastasis cascade: local invasion, one or more early post-intravasation events, and metastatic colonization (Valastyan et al., 2009). Such pleiotropy provides a rationale for the high frequency with which this complex series of events is accomplished over the course of a typical human lifespan.
Hence, via the accumulation of genetic and/or epigenetic alterations – as well as the co-option of non-neoplastic stromal cells – carcinoma cells are capable of completing an intricate, multi-step, cell-biological process that culminates in the formation of macroscopic, life-threatening growths at distant organ sites.
Metastasis is a Highly Inefficient Process
As might be logically inferred from the preceding discussions, the invasion-metastasis cascade is extraordinarily inefficient. For example, large numbers of CTCs can be detected within the bloodstream of the overwhelming majority of carcinoma patients, including those who develop few – if any – overt metastases (Nagrath et al., 2007). In fact, some have estimated that <0.01% of tumor cells that enter into the systemic circulation ultimately develop into macroscopic metastases (Chambers et al., 2002), and this may represent an over-estimate.
This point was vividly demonstrated by observing 15 ovarian cancer patients who were provided palliative remediation of their peritoneal ascites via the installation of peritoneovenous shunts. In addition to relieving discomfort, this treatment – which evacuates ascitic fluid directly into the venous circulation – continuously liberated millions of cancer cells into their systemic circulation. Nevertheless, these patients largely failed to develop detectable metastases even several years later (Tarin et al., 1984). Taken together, these observations suggest that one or more of the later steps of the invasion-metastasis cascade – namely, survival in the circulation, arrest at distant sites, extravasation, initial survival in foreign microenvironments, and/or metastatic colonization – are successfully completed only very infrequently.
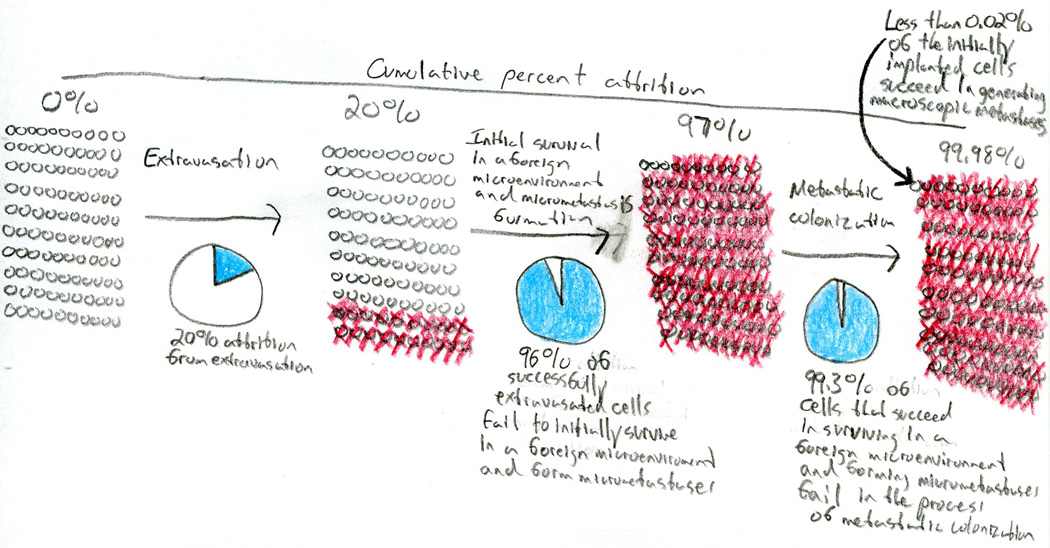
In fact, detailed work in experimental models has further defined the particular steps of metastasis that appear to be rate-limiting. More specifically, survival in the circulation, arrest at distant sites, and extravasation occur quite efficiently in various carcinoma cell types (e.g., >80% of intravenously implanted cells succeed in extravasating). In contrast, once tumor cells exited the microvasculature into the parenchyma of foreign tissues, high rates of attrition are observed (e.g., <3% of intravenously implanted cells survive to form micrometastases). Importantly, although a substantial proportion of successfully extravasated tumor cells failed to initially survive within distant tissue sites to generate micrometastases, the subsequent process of metastatic colonization is even more inefficient – perhaps by several orders of magnitude (e.g., <0.02% of intravenously implanted cells generate macroscopic metastases) (Figure 5) (Luzzi et al., 1998). Collectively, these findings converge on the conclusion that metastatic colonization often represents the dominant rate-limiting step of the invasion-metastasis cascade.
Figure 5. Inefficiency of the Invasion-Metastasis Cascade: Metastatic Colonization is Often Rate-Limiting.
Certain steps of the invasion-metastasis cascade are successfully completed with only extraordinary inefficiency. Work in experimental models has revealed that the process of metastatic colonization typically represents the rate-limiting step of the invasion-metastasis cascade, with a rate of attrition that often exceeds 99% of those cells that initially survive in a foreign microenvironment to form micrometastases. Red x-marks denote the approximate cumulative fraction of intravenously implanted tumor cells that have died after passage through the indicated steps of the invasion-metastasis cascade.
Consistent with this notion, among 1438 breast carcinoma patients who harbored hundreds to thousands of micrometastases in their bone marrow at the time of initial diagnosis, only 50% developed clinically detectable metastases within 10 years (Braun et al., 2005). Further support for the belief that metastatic colonization frequently represents the rate-limiting step of the invasion-metastasis cascade comes from clinical observations describing the kinetics of distant relapse and disease recurrence. In many human tumor types – for example, breast carcinomas – detectable metastases often arise years or even decades after the apparent complete resection of a patient’s primary tumor (Aguirre-Ghiso, 2007). Because the metastatic cells must have disseminated from the primary tumor prior to its surgical removal, this implies that these cells persisted in an occult yet viable state for many years at anatomically distant organ sites. The most parsimonious interpretation of these clinical observations is that, although the incipient metastatic precursor cells were capable of disseminating and retaining viability at distant loci, the appearance of detectable metastases was greatly delayed due to the gross inefficiency of metastatic colonization. Ostensibly, during this long period of latency, a small minority of disseminated carcinoma cells underwent gradual genetic and/or epigenetic evolution in order to acquire the adaptive traits required for metastatic colonization.
Importantly, certain human tumor types – notably lung and pancreatic adenocarcinomas – do not display characteristic years- or decades-long latency periods prior to overt metastasis formation. Instead, these tumors progress rapidly to macroscopic metastases upon infiltration of distant organ sites (Nguyen et al., 2009). Such clinical observations suggest that lung and pancreatic adenocarcinoma cells exiting their primary sites of growth are already reasonably well-equipped to generate macroscopic metastases – possibly due, at least in part, to the differentiation programs of the normal epithelial cells from which these neoplasias were derived. These findings fail, however, to provide insight regarding the specific rate-limiting step(s) of the invasion-metastasis cascade in these particular tumor types, since the relative efficiency of the various steps of metastasis in lung and pancreatic adenocarcinomas remain largely unexplored.
Despite the high rates of attrition that accompany certain steps of the invasion-metastasis cascade, overt metastases do eventually arise in many carcinoma patients – where they almost invariably represent the source of terminal disease (Gupta and Massagué, 2006). These points draw attention to questions regarding the origins of the cells that serve as precursors of overt metastases, as well as the timing of – and the anatomical sites at which – the genetic and/or epigenetic events that drive the molecular evolution of these cells toward metastatic competence transpire.
How, When, and Where Do the Precursor Cells of Overt Metastases Arise During the Course of Tumor Progression?
The notion that tumor cell populations evolve via a process akin to Darwinian selection has found widespread acceptance. Stated simply, this model posits that genetic variation is continually introduced into the population via stochastic mutational events, and that those cell clones that happen to acquire alleles conferring proliferative and/or survival advantages become overrepresented via a process of purifying selection. Thereafter, these new, genetically altered populations become the substrates for subsequent rounds of mutation and clonal selection. In recent years, this Darwinian model has been expanded to include heritable cellular traits that are acquired via epigenetic mechanisms (Gupta and Massagué, 2006).
However, the Darwinian model must somehow accommodate conclusions flowing from the preceding discussions, which indicated that (1) the molecular and cell-biological requirements for carcinoma cells to thrive at primary sites versus metastatic sites can be very different and (2) metastatic colonization is often and perhaps always the rate-limiting step of the invasion-metastasis cascade. These considerations raise the question of how, according to the Darwinian selection model, cell clones that possess traits enabling them to form metastases in specific distant organ sites arise within primary tumors.
In some instances, the answer may be somewhat trivial: certain molecular changes can confer acquired abilities that promote proliferation and/or survival at both primary and metastatic sites. Genes whose altered activities participate in tumor pathogenesis in this manner have been termed “metastasis initiation genes” or “metastasis progression genes” (Nguyen et al., 2009). In the case of pleiotropically acting regulatory factors, the biochemical functions responsible for endowing these growth-promoting attributes may differ between primary tumors and foreign microenvironments; nevertheless, selection for heightened activity of the factor in the context of primary tumor development may inadvertently benefit growth at a distant organ site.
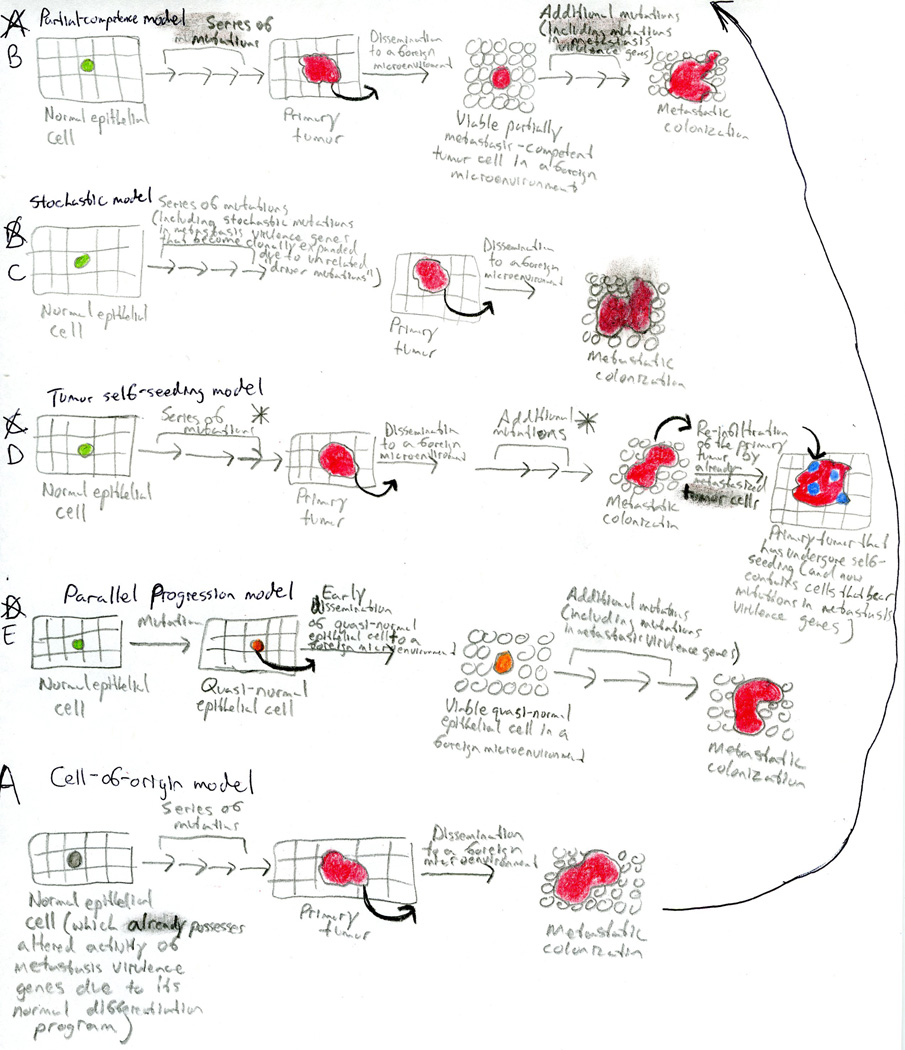
More puzzling is the problem of how cells expressing “metastasis virulence genes” – genetic factors that fail to affect primary tumor development and confer proliferation and/or survival advantages only within the context of specific foreign microenvironments (Nguyen et al., 2009) – can arise at appreciable frequencies during the course of malignant progression. Because the altered activity of these genes does not – by definition – impact primary tumor development, cancer cells expressing these factors cannot be selected during the evolution of primary tumors. Nevertheless, in light of the fact that metastatic disease often involves the aberrant activity of metastasis virulence genes, it is clear that cells bearing these molecular alterations do arise at reasonably high frequencies at some point during malignant progression. The expression of some of these genes may reflect the continuing influence of the differentiation programs of the cells-of-origin from which certain primary tumors are derived (Figure 6A).
Figure 6. Models to Explain the Acquisition of Molecular Alterations in Metastasis Virulence Genes.
A number of models have recently been proposed in order to explain how tumor cell populations evolve to acquire molecular alterations in metastasis virulence genes. (A) The normal differentiation programs of the cells-of-origin from which certain primary tumors are derived may already dictate the altered activity of various metastasis virulence genes (depicted in gray). Upon subsequent oncogenic transformation and systemic dissemination, these cells may therefore be capable of completing the process of metastatic colonization. (B) Cells that are only partially metastasis-competent (i.e., tumor cells that have acquired a series of mutations that confer the capacity to disseminate systemically, but are initially unable to colonize foreign microenvironments) may arrive at distant organs, where they then undergo further genetic and/or epigenetic evolution within these foreign microenvironments in order to achieve full metastatic competence. Such molecular evolution would likely include alterations in metastasis virulence genes. (C) Purely by chance, mutations in metastasis virulence genes may accumulate stochastically as “passenger mutations” within tumor cell clones that bear unrelated “driver mutations” that serve to fuel the clonal expansion of these cells within primary tumors. (D) The phenomenon of tumor self-seeding indicates that already-metastasized cells are capable of re-infiltrating the primary tumor from which they originated. Hence, carcinoma cells present in metastases (which have come to acquire molecular alterations in metastasis virulence genes via either of the models proposed above – as indicated by the asterisk) may become increasingly represented within their primary-tumor-of-origin (re-infiltrating cells are depicted in blue). (E) The parallel progression model asserts that quasi-normal epithelial cells (depicted in orange) disseminate very early from pre-neoplastic lesions. Subsequently, these cells undergo molecular evolution at future sites of metastasis formation. Notably, such sites represent locations where mutations in metastasis virulence genes are now selectively advantageous. Carcinoma cells are depicted in red.
In addition, cells may arise in the primary tumor that are only partially metastasis-competent (i.e., tumor cells that have undergone molecular changes that render them capable of disseminating to distant sites, but that still require additional molecular changes in order to successfully colonize those organs). Upon dissemination to distant organs, these cells may undergo additional genetic and/or epigenetic evolution in these foreign tissue microenvironments – sites where the acquisition of alterations in metastasis virulence genes are indeed selectively advantageous (Figure 6B).
An alternative model explaining the acquisition of metastasis virulence genes involves the stochastic accumulation of molecular changes in such genes during primary tumor evolution. For example, mutations in metastasis virulence genes may be acquired as “passenger mutations” within highly mutable tumor cell populations that possess unrelated “driver mutations” (Stratton, 2011), the latter serving to drive the clonal expansion of these cells within primary tumors. Accordingly, purely by chance, subpopulations of cells within primary tumors may inadvertently acquire mutations in metastasis virulence genes and thus possess high proclivities to metastasize (Figure 6C).
A fourth explanation is provoked by the phenomenon of “tumor self-seeding”. This mechanism was formulated based on observations of xenograft models of breast and colon carcinomas, where it was demonstrated that carcinoma cells present in metastases are capable of re-infiltrating their primary-tumor-of-origin (Kim et al., 2009). If primary tumors successfully spawn metastases in distant organs, and if already-metastasized cells are capable of re-seeding the primary tumors from which they arose, then it becomes possible that these primary tumors will progressively acquire the molecular signatures of the metastases that they have previously spawned. This would include changes in metastasis virulence genes that may have been selected while the disseminated cells were evolving at distant organ sites or that accumulated via stochastic mechanisms (Figure 6D).
While it has been widely assumed that the majority of malignant progression occurs within primary tumors, a recent proposal suggests something quite different – that this genetic evolution can instead occur largely at sites that are distant from primary tumors, resulting in the acquisition of genes that enable both tumorigenicity and metastatic virulence. According to this thinking, quasi-normal cells may disseminate from pre-neoplastic lesions relatively early during the course of tumor progression. Independent of the molecular evolution that is occurring in the corresponding primary tumor, these quasi-normal cells are then proposed to undergo multiple rounds of genetic diversification followed by clonal selection within the distant organ sites in which overt metastases ultimately develop – specifically, microenvironments where mutations in metastasis virulence genes can now be selectively advantageous (Figure 6E) (Klein, 2009). This so-called “parallel progression model” (in contrast to the traditional “linear progression model” of carcinoma metastasis described above) was recently proposed in light of several independent observations from human breast carcinoma patients and experimental mammary tumor models: (1) cells that are not yet fully neoplastic are routinely disseminated in a systemic manner from even early pre-malignant lesions (Nagrath et al., 2007; Hüsemann et al., 2008), (2) untransformed epithelial cells present in the systemic circulation can survive within the vasculature, arrest at distant organ sites, extravasate, and survive in foreign microenvironments for prolonged intervals (Podsypanina et al., 2008), (3) early-disseminating pre-neoplastic cells possess at least some capacity for cell proliferation at distant organ sites (Hüsemann et al., 2008; Podsypanina et al., 2008), and (4) patient-matched primary tumors and metastases can harbor significantly different spectra of molecular alterations (Schmidt-Kittler et al., 2003). Thus, it is possible that largely normal breast epithelial cells that disseminate relatively early during the course of tumor progression can represent the precursor cells of overt metastases, owing to their gradual evolution at sites of eventual metastasis formation.
Importantly, the parallel progression model is not disproved by observations that expression signatures predictive of propensity for metastatic relapse can be identified via microarray analysis of breast carcinoma patient primary tumors (van’t Veer et al., 2002; Ramaswamy et al., 2003; Paik et al., 2004). This is because these “metastasis signatures” could, in actuality, represent “dissemination signatures” that facilitate the escape of not-yet fully neoplastic cells to distant organ sites, where they would then serve as substrates for additional rounds of Darwinian selection.
Instead, the major conceptual problem that must be addressed by the parallel progression model concerns how these disseminated quasi-normal mammary cells can actually evolve in distant organ sites. Both genetic and epigenetic evolution would appear to require repeated rounds of cell division in order to generate the genetic and phenotypic diversity that yields novel cell populations with increased fitness. However, these disseminated quasi-normal cells confront major obstacles to their proliferation, as even cancer cells that are fully neoplastic have extremely low chances of actively proliferating at sites of dissemination, and the proliferation of quasi-normal cells is further handicapped by the fact that these cells lack many of the mutant genes that are required to drive active cell proliferation in the primary tumor site.
Additionally, while some studies have documented extensive molecular differences between patient-matched primary breast tumors and metastases (Schmidt-Kittler et al., 2003), many other investigators have found metastases and their corresponding primary breast tumors to be quite similar (Ramaswamy et al., 2003; Weigelt et al., 2003; Ding et al., 2010; Navin et al., 2011). Moreover, whole-genome sequencing of 20 patient-matched primary pancreatic tumors and metastases documented that the majority of genomic alterations present in the metastases were also present in the corresponding primary tumors (Campbell et al., 2010; Yachida et al., 2010). An analogous conclusion was reached by sequencing 289 candidate exons in 10 patient-matched primary colorectal carcinomas and metastases (Jones et al., 2008). Finally, genomic analyses of patient-matched primary prostate tumors and metastases revealed that the metastases bear the copy-number signature of the primary tumor from which they were initially spawned (Liu et al., 2009). These molecular analyses make it unlikely that the precursor cells of overt metastases in pancreatic, colorectal, and prostate carcinomas disseminate early to sites where they proceed to undergo their own divergent genetic evolution.
In essence, while it now appears clear that quasi-normal breast cells can enter into the systemic circulation early during the course of tumor progression, direct evidence implicating these early-disseminating cells as the precursors of overt metastases remains scant. Nonetheless, if ultimately proven correct, the parallel progression model would necessitate a paradigm shift and would hold serious implications for the design of effective therapeutic agents aimed at treating metastatic disease.
Emerging Clinical Opportunities to Target Metastatic Disease
Of critical importance is the question of whether insights gleaned from basic laboratory research will prove useful to the diagnosis and treatment of clinical metastatic disease. Because, as mentioned earlier, metastases are responsible for approximately 90% of cancer-associated patient mortality, truly informative prognostic biomarkers and novel therapeutic targets represent areas of great need.
Prognostic Biomarkers
Research conducted over the past decade has succeeded in identifying a number of biomarkers whose levels in primary breast tumors are associated with the propensity of a patient to suffer metastatic relapse. Some of these biomarkers have been subjected to extensive independent validation and have entered into clinical use – for example, the MammaPrint and Oncotype DX assays (van’t Veer et al., 2002; Paik et al., 2004). These assays employ multi-gene expression signatures to estimate the likelihood of disease progression and recurrence, and then utilize this information to direct adjuvant treatment options. Interestingly, while the specific genes that comprise these two prognostic signatures are almost entirely non-overlapping, applying these two assays to an individual tumor specimen yields a concordant prediction in >80% of cases (Fan et al., 2006). Such findings suggest that these two signatures identify a common set of biological outputs. At the same time, the minimal overlap between these two sets of genes lessens the likelihood that the particular genes included in these assays represent functionally critical mediators of metastatic progression.
Importantly, these assays are principally informative for the prognosis of patients within only certain subclasses of primary breast tumors and fail to identify individuals with heightened risk who suffer from other subtypes of the disease (Desmedt et al., 2008). Therefore, refinement of prognostic signatures is required in order to increase further their power to predict metastatic relapse. With the passage of time, the need for such improvement has become increasingly acute: it is now clear that the majority of women who are diagnosed with breast cancer carry a form of the disease that is highly unlikely to generate life-threatening metastases; nonetheless, these women are treated as aggressively as those whose tumors carry truly grim prognoses, resulting in enormous unnecessary exposure of these women to the toxicities of anti-neoplastic therapies.
One possible avenue of improvement in prognosis comes from the discovery that miRNAs play critical mechanistic roles in a wide variety of normal and pathological processes. This suggests their potential utility to yield useful biomarkers of metastatic propensity. Indeed, the levels of several individual miRNAs – including miR-10b, miR-21, miR-31, miR-126, miR-335, and miR-373 – have been correlated with metastatic outcome in carcinoma patients (Valastyan and Weinberg, 2009). In fact, miRNA expression signatures have proven to be even more useful than the corresponding mRNA profiles at stratifying primary tumors based on their tissue-of-origin (Lu et al., 2005), and multi-gene miRNA expression signatures predictive of metastatic outcome have now been assembled (Yu et al., 2008). Additionally, other classes of non-coding RNAs – including large intervening non-coding RNAs (lincRNAs) such as HOTAIR (Gupta et al., 2010) – have also been proposed as putative biomarkers for metastatic propensity in human breast tumors. The application of miRNA or lincRNA expression arrays to prognosis in the oncology clinic has yet to occur.
As of late, the development of instruments that detect CTCs offers yet another prospect for developing a useful prognostic parameter. Overall numbers of CTCs in patients afflicted with any of a variety of carcinoma types provide a prognostic indicator of disease outcome (Pantel et al., 2008). Moreover, changes in CTC levels upon administration of neo-adjuvant or adjuvant therapeutic agents may provide a minimally invasive means by which to rapidly gauge patient-responsiveness to these drug treatments (Cristofanilli et al., 2004). It is worth noting, however, that the prognostic significance of CTC numbers may not be universally applicable (Pantel et al., 2008), and future work is necessary to determine the criteria under which quantification of CTCs provides additional information about patient outcome beyond that generated by currently employed diagnostic modalities. Moreover, at present, many of the devices that measure CTC numbers rely on the expression of epithelial cell-surface molecules by the tumor cells; consequently, these analyses are ostensibly unable to detect subpopulations of CTCs that have, for example, undergone an EMT and thus shed epithelial markers. Nevertheless, CTC detection platforms – as well as, perhaps, direct detection of tumor-specific molecular alterations in freely circulating nucleic acids present in the bloodstream (Schwarzenbach et al., 2011) – may come to represent important clinical tools for diagnosing and guiding the treatment of metastatic disease.
Therapeutic Agents
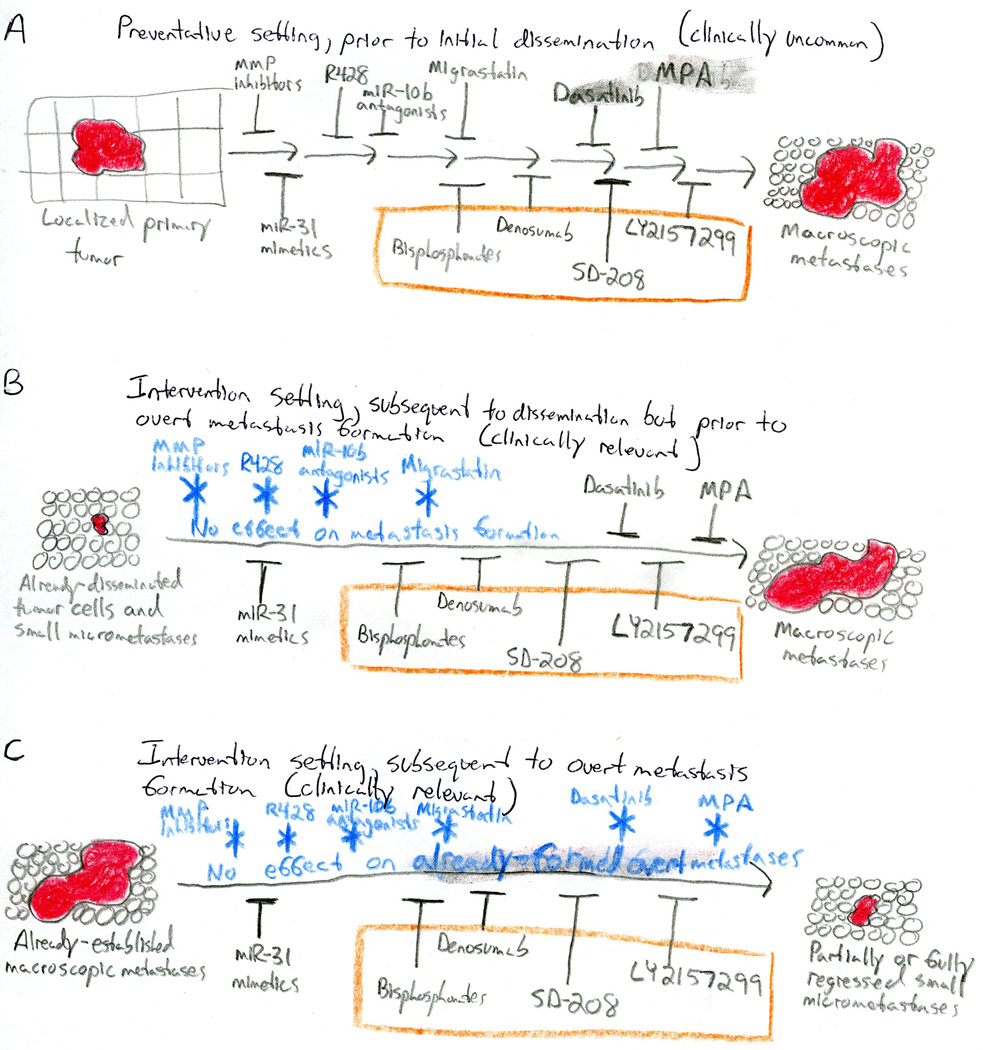
A key consideration in the design of anti-metastatic therapeutic agents is the fact that carcinoma patients frequently already harbor significant numbers of disseminated tumor cells in their blood, bone marrow, and distant organ sites upon initial presentation in the oncology clinic (Braun et al., 2005; Nagrath et al., 2007; Pantel et al., 2008). Consequently, truly effective anti-metastatic therapeutics must be capable of impairing the proliferation and survival of already-disseminated carcinoma cells, rather than merely attempting to block escape of these cells from primary tumors (Figure 7). Unfortunately, however, the rationale behind many targeted agents that were designed to impair carcinoma metastasis – such as MMP inhibitors, the Axl kinase inhibitor R428, miR-10b antagonists, and the fascin inhibitor Migrastatin – is incompatible with these clinical observations, as these compounds are believed to act principally by impairing initial dissemination events (Kessenbrock et al., 2010; Holland et al., 2010; Ma et al., 2010; Chen et al., 2010).
Figure 7. Rationally Designed Therapeutic Agents Intended for the Remediation of Metastatic Disease.
Because metastases are culpable for >90% of cancer-associated mortality, truly efficacious anti-metastatic therapies are desperately needed. (A) Various rationally designed anti-metastatic compounds trigger measurable responses in pre-clinical preventative settings where treatment is initiated prior to the formation of primary tumors or metastases. (B) Unfortunately, however, many agents that display efficacy in preventative pre-clinical models fail to impair metastasis in pre-clinical intervention settings where treatment is initiated only after the formation of small micrometastases (depicted in blue). Because carcinoma patients frequently already harbor significant numbers of disseminated tumor cells at the time of initial disease presentation, the ultimate translational utility of compounds that are unable to alter the behavior of already-formed metastases is likely be quite limited. In contrast, dasatinib, medroxyprogesterone acetate (MPA), miR-31 mimetics, bisphosphonates, denosumab, SD-208, and LY2157299 inhibit the metastatic outgrowth of already-disseminated tumor cells in intervention assays (depicted in gray). (C) In the end, agents that are capable of eliciting the regression of already-established macroscopic metastases may possess the greatest clinical utility. Compounds displaying such efficacy in pre-clinical intervention settings are quite rare, though several examples have been reported – namely, miR-31 mimetics, bisphosphonates, denosumab, SD-208, and LY2157299. In contrast, many other compounds are incapable of altering the behavior of already-established macroscopic metastases (indicated in blue) – including agents that display efficacy against small micrometastases prior to their overt metastatic colonization. Carcinoma cells are depicted in red. Therapeutic agents whose mechanism of action is believed to principally involve the targeting of non-neoplastic stromal cells are presented within the orange boxes. MMP: matrix metalloproteinase; MPA: medroxyprogesterone acetate.
If anti-metastatic drugs do not additionally impact the behavior of already-established metastases, then their ultimate clinical utility will likely be confined to long-term prophylactic settings; such use in the clinic is unlikely, because of the almost-inevitable side-effects of essentially all agents. Thus, the limited benefit – as well as severe adverse side-effects – observed in clinical trials involving MMP inhibitors is not encouraging (Kessenbrock et al., 2010). Moreover, pre-clinical studies reveal that R428, miR-10b antagonists, and Migrastatin fail to affect the fates of already-disseminated tumor cells (Holland et al., 2010; Ma et al., 2010; Oskarsson et al., 2010). Nevertheless, it may be premature to entirely discount these and similar compounds as potential therapeutic agents against clinical disseminated disease, as pre-clinical model systems often do not adequately recapitulate latent metastatic disease or reactivated metastatic showers. Moreover, it remains possible that better, more specific MMP inhibitors might exhibit enhanced efficacy and reduced toxicity.
Importantly, existing therapies designed to destroy primary tumors – both general cytotoxic agents and rationally designed targeted compounds – often display only limited activity against the corresponding metastatic lesions (Steeg, 2006). This lack of efficacy could reflect physical limitations related to drug delivery, dictated by either poor vascularization of metastatic nodules or by anatomical locations of target organs (e.g., the blood-brain barrier that may protect brain metastases from therapeutic agents delivered via the hematogenous circulation) (Carmeliet and Jain, 2011). Indeed, certain metastatic sites may afford chemoprotective niches (Gilbert and Hemann, 2010).
It is also likely that occult, slowly growing micrometastases can resist the effects of cytotoxic agents that principally target cells in their active growth-and-division cycle (Aguirre-Ghiso, 2007). Furthermore, primary tumors and their derived metastases may be molecularly distinct from one another, rendering certain therapeutic strategies directed against the genotypes of primary tumors ineffective against their corresponding metastases (Klein, 2009). It is also possible that the neoplastic cells within metastases are intrinsically more drug-resistant than are cells in the corresponding primary tumors; additional molecular changes occurring within the disseminated cells – perhaps involving acquisition of TIC-like properties – have been cited as one possible source of such heightened resistance (Thiery et al., 2009). Collectively, the preceding observations explain why truly effective anti-metastatic therapeutics have yet to enter into clinical practice.
Collectively, these findings further reinforce the importance of developing novel agents that are capable of affecting the proliferation and survival of already-established metastases. As an example of such a compound, the Src inhibitor dasatinib inhibits the formation of bone metastases by breast carcinoma cells in xenograft models, doing so via impairing the survival of already-extravasated tumor cells prior to overt colonization of the marrow (Zhang et al., 2009). Additionally, transcriptional activation of a suppressor of metastatic colonization, non-metastatic cells protein 23 (NM23), in already-disseminated breast carcinoma cells – achieved via administration of the NM23 transcriptional activator medroxyprogesterone acetate (MPA) – diminished both the overall numbers and relative sizes of metastatic foci in tumor-bearing mice (Palmieri et al., 2005). These pre-clinical studies principally evaluated the consequences of perturbing Src or NM23 function in already-seeded micrometastases. Such an experimental setting may serve as a reasonable model of the minimal-residual-disease state often encountered in carcinoma patients following primary tumor resection, but does not address the more serious clinical problem of treating already-robustly growing macroscopic metastases.
In the end, the greatest translational therapeutic utility will derive from agents that actively trigger the regression of established macroscopic metastatic foci. For example, pre-clinical studies have evaluated the consequences of acutely expressing the miRNA miR-31 – a pleiotropically acting suppressor of local invasion, early post-intravasation events, and metastatic colonization – in already-formed metastases generated by breast carcinoma cells. Acute expression of miR-31 in already-disseminated tumor cells not only prevented the outgrowth of established micrometastases, but also elicited the regression of already-robustly growing macroscopic metastases. These effects appear to be orchestrated through metastasis-specific suppression of Akt-mediated signaling and induction of the pro-apoptotic molecule Bim (Valastyan et al., 2011). Therefore, these observations begin to suggest that miR-31 mimetics may possess the properties of a truly useful anti-metastatic agent of the future.
The therapeutic strategies cited above are focused on targeting the “seeds” (i.e., tumor cells themselves); however, effective anti-metastatic responses can also be achieved via delivery of compounds that alter the “soil” of the foreign tissue microenvironments present at metastatic sites. For example, bisphosphonates – as well as the anti-RANK antibody denosumab and various TGFβ inhibitors like SD-208 and LY2157299 – have been proposed as inhibitors of bone metastasis in patients afflicted with breast and lung carcinomas. These compounds prevent osteoclast-mediated degradation of bone, an event that contributes to the pathogenesis of bone metastatic colonization. Notably, bisphosphonates and denosumab alter the proliferation and survival of already-disseminated tumor cells in experimental models. Moreover, early results from clinical trials suggest that bisphosphonates may lower the risk of bone metastasis in high-risk individuals, as well as increase overall patient survival (Weilbaecher et al., 2011). These successes in targeting the non-neoplastic stromal cells that metastatic carcinoma cells require when attempting to colonize the bone provide a strong impetus for devising analogous strategies that target stromal cell types involved in the metastatic colonization of other organ sites.
One such stromal cell type that has long been considered to represent a viable target for anti-metastatic therapeutics are the endothelial cells that provide vascularization to growing metastatic nodules. However, the provocative observation that VEGF-targeting anti-angiogenic compounds paradoxically increase metastatic propensity in murine models has provided a cautionary tale regarding the possibly unanticipated effects on metastases of these agents (Ebos et al., 2009; Páez-Ribes et al., 2009). However, other pre-clinical studies failed to document increased metastasis upon treatment with VEGF-targeting agents (Padera et al., 2008). Importantly, retrospective analysis of 4205 human patients with breast, colorectal, renal, or pancreatic carcinomas who were treated with the anti-VEGF compound bevacizumab did not reveal an association of bevacizumab treatment with either enhanced disease progression or increased mortality (Miles et al., 2011). In light of these conflicting data, further studies investigating the effects of anti-angiogenic compounds on the behavior of metastases appear merited.
Together, the above discussions illustrate that while numerous clinically useful prognostic biomarkers for metastatic propensity have been identified in recent years, the discovery of effective anti-metastatic therapeutics has lagged behind. Nonetheless, the increased appreciation that anti-metastatic therapeutics must target already-established metastases and the impressive recent progress cited earlier concerning various mechanisms that control metastatic colonization, give cause for optimism moving forward. Importantly, however, in light of their potentially metastasis-specific effects, clinical development of these putative metastatic colonization-targeting therapeutic agents of the future will almost certainly require significant re-evaluation of traditional clinical trial benchmarks and study endpoints.
Concluding Remarks and Future Perspective
Although a number of fundamental questions concerning the basic nature of carcinoma metastasis remain incompletely understood, recent research has succeeded in implicating specific molecules in the regulation of discrete cell-biological aspects of the invasion-metastasis cascade. Moreover, the roles played by stromal cells during each step of the metastatic process are rapidly beginning to be appreciated. In many instances, this work has revealed unanticipated complexities and forced revision of established conceptual frameworks.
Looking ahead, we envision that technological advances will continue to revolutionize cancer biology and the study of metastasis. For example, improved imaging platforms have facilitated previously unimaginable real-time visualization of the metastatic process in vivo (Sahai, 2007). Additionally, an improved molecular toolkit will permit more extensive evaluation of the heterogeneity that exists within tumor cell populations, as well as interrogation of its functional significance. Of relevance to this matter, it has been reported that admixing two non-metastatic subpopulations of small cell lung cancer cells enables robust metastasis formation due to incompletely understood pro-malignant crosstalk between these distinct subclones (Calbo et al., 2011). Also of interest, the observation that certain carcinoma cells are capable of trans-differentiating into bona fide endothelial cells that are competent to contribute to the tumor neovasculature suggests a previously unexpected level of plasticity and functional heterogeneity within tumor cell populations and their associated stromal compartments (Ricci-Vitiani et al., 2010; Wang et al., 2010).
Metastasis research has entered into a stage of remarkable progress. Over the past five years, our comprehension of the pathways that orchestrate the invasion-metastasis cascade has evolved from almost-total ignorance to a detailed molecular circuitry diagram endowed with clear central control nodes. Consequently, we envisage that metastatic behavior will increasingly be understood to arise through a finite number of organizing principles. In light of the dire clinical realities associated with metastatic disease, we cannot overstate the importance of ensuring that this impressive pace of discovery continues – and, additionally, is accompanied by the rapid translation of these basic research findings to the oncology clinic.
ACKNOWLEDGMENTS
We apologize to the many individuals whose valuable contributions to metastasis research were unable to be cited due to space restrictions. We thank Joan Brugge, Julie Valastyan, Wenjun Guo, and Sandra McAllister for critical review of this manuscript, as well as Eva Valastyan for helpful discussions. Research in the authors’ laboratories is supported by the NIH, MIT Ludwig Center for Molecular Oncology, U.S. Department of Defense, and Breast Cancer Research Foundation. S.V. is a Damon Runyon Fellow supported by the Damon Runyon Cancer Research Foundation. R.A.W. is an American Cancer Society Research Professor and a Daniel K. Ludwig Foundation Cancer Research Professor.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Aguirre-Ghiso JA. Models, mechanisms, and clinical evidence for cancer dormancy. Nat Rev Cancer. 2007;7:834–846. doi: 10.1038/nrc2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Mehdi AB, Tozawa K, Fisher AB, Shientag L, Lee A, Muschel RJ. Intravascular origin of metastasis from the proliferation of endothelium-attached tumor cells: a new model for metastasis. Nat Med. 2000;6:100–102. doi: 10.1038/71429. [DOI] [PubMed] [Google Scholar]
- Auguste P, Fallavollita L, Wang N, Burnier J, Bikfalvi A, Brodt P. The host inflammatory response promotes liver metastasis by increasing tumor cell arrest and extravasation. Am J Pathol. 2007;170:1781–1792. doi: 10.2353/ajpath.2007.060886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkan D, El Touny LH, Michalowski AM, Smith JA, Chu I, Davis AS, Webster JD, Hoover S, Simpson RM, Gauldie J, et al. Metastatic growth from dormant cells induced by col-I-enriched fibrotic environment. Cancer Res. 2010;70:5706–5716. doi: 10.1158/0008-5472.CAN-09-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkan D, Kleinman H, Simmons JL, Asmussen H, Kamaraju AK, Hoenorhoff MJ, Liu ZY, Costes SV, Cho EH, Lockett S, et al. Inhibition of metastatic outgrowth from single dormant tumor cells by targeting the cytoskeleton. Cancer Res. 2008;68:6241–6250. doi: 10.1158/0008-5472.CAN-07-6849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bissell M, Hines WC. Why don’t we get more cancer? A proposed role of the microenvironment in restraining cancer progression. Nat Med. 2011;17:320–329. doi: 10.1038/nm.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos PD, Zhang XH, Nadal C, Shu W, Gomis RR, Nguyen DX, Minn AJ, van de Vijver MJ, Gerald WL, Foekens JA, et al. Genes that mediate breast cancer metastasis to the brain. Nature. 2009;459:1005–1009. doi: 10.1038/nature08021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Coombes RC, Schlimok G, Diel IJ, Gerber B, Gebauer G, et al. A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med. 2005;353:793–802. doi: 10.1056/NEJMoa050434. [DOI] [PubMed] [Google Scholar]
- Brown DM, Ruoslahti E. Medadherin, a cell surface protein in breast tumors that mediates lung metastasis. Cancer Cell. 2004;5:365–374. doi: 10.1016/s1535-6108(04)00079-0. [DOI] [PubMed] [Google Scholar]
- Calbo J, van Montfort E, Proost N, van Drunen E, Beverloo HB, Meuwissen R, Berns A. A functional role for tumor cell heterogeneity in a mouse model of small cell lung cancer. Cancer Cell. 2011;19:244–256. doi: 10.1016/j.ccr.2010.12.021. [DOI] [PubMed] [Google Scholar]
- Campbell PJ, Yachida S, Mudie LJ, Stephens PJ, Pleasance ED, Stebbings LA, Morsberger LA, Latimer C, McLaren S, Lin ML, et al. The patterns and dynamics of genomic instability in metastatic pancreatic cancer. Nature. 2010;467:1109–1113. doi: 10.1038/nature09460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmeliet P, Jain RK. Principles and mechanisms of vessel normalization for cancer and other angiogenic diseases. Nat Rev Drug Discov. 2011;10:417–427. doi: 10.1038/nrd3455. [DOI] [PubMed] [Google Scholar]
- Chambers AF, Groom AC, MacDonald IC. Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer. 2002;2:563–572. doi: 10.1038/nrc865. [DOI] [PubMed] [Google Scholar]
- Chang HY, Sneddon JB, Alizadeh AA, Sood R, West RB, Montgomery K, Chi JT, van de Rijn M, Bostein D, Brown PO. Gene expression signature of fibroblast serum response predicts human cancer progression: similarities between tumors and wounds. PLoS Biol. 2004;2:E7. doi: 10.1371/journal.pbio.0020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Yang S, Jakoncic J, Zhang JJ, Huang X. Migrastatin analogues target fascin to block tumour metastasis. Nature. 2010;464:1062–1066. doi: 10.1038/nature08978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clevers H. The cancer stem cell: premises, promises and challenges. Nat Med. 2011;17:313–319. doi: 10.1038/nm.2304. [DOI] [PubMed] [Google Scholar]
- Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med. 2004;351:781–791. doi: 10.1056/NEJMoa040766. [DOI] [PubMed] [Google Scholar]
- Dawson MR, Duda DG, Fukumura D, Jain RK. VEGFR1-activity-independent metastasis formation. Nature. 2009;461:E4–E5. doi: 10.1038/nature08254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeNardo DG, Barreto JB, Andreu P, Vasquez L, Tawfik D, Kolhatkar N, Coussens LM. CD4+ cells regulate pulmonary metastasis of mammary carcinomas by enhancing protumor properties of macrophages. Cancer Cell. 2009;16:91–102. doi: 10.1016/j.ccr.2009.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desmedt C, Haibe-Kains B, Wirapati P, Buyse M, Larsimont D, Bontempi G, Delorenzi M, Piccart M, Sotiriou C. Biological processes associated with breast cancer clinical outcome depend on the molecular subtypes. Clin Cancer Res. 2008;14:5158–5165. doi: 10.1158/1078-0432.CCR-07-4756. [DOI] [PubMed] [Google Scholar]
- Ding L, Ellis MJ, Li S, Larson DE, Chen K, Wallis JW, Harris CC, McLellan MD, Fulton RS, Fulton LL, et al. Genome remodelling in a basal-like breast cancer metastasis and xenograft. Nature. 2010;464:999–1005. doi: 10.1038/nature08989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirat B, Bochet L, Dabek M, Daviaud D, Dauvillier S, Majed B, Wang YY, Meulle A, Salles B, Le Gonidec S, et al. Cancer-associated adipocytes exhibit an activated phenotype and contribute to breast cancer invasion. Cancer Res. 2011;71:2455–2465. doi: 10.1158/0008-5472.CAN-10-3323. [DOI] [PubMed] [Google Scholar]
- Douma S, Van Laar T, Zeyenhoven J, Meuwissen R, Van Garderen E, Peeper DS. Suppression of anoikis and induction of metastasis by the neurotrophic receptor TrkB. Nature. 2004;430:1034–1039. doi: 10.1038/nature02765. [DOI] [PubMed] [Google Scholar]
- Ebos JML, Lee CR, Cruz-Munoz W, Bjarnason GA, Christensen JG, Kerbel RS. Accelerated metastasis after short-term treatment with a potent inhibitor of tumor angiogenesis. Cancer Cell. 2009;15:232–239. doi: 10.1016/j.ccr.2009.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erler JT, Bennewith KL, Cox TR, Lang G, Bird D, Koong A, Le QT, Giaccia AJ. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell. 2009;15:35–44. doi: 10.1016/j.ccr.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan C, Wessels L, Weigelt B, Nuyten DS, Nobel AB, van’t Veer LJ, Perou CM. Concordance among gene-expression-based predictors for breast cancer. N Engl J Med. 2006;355:560–569. doi: 10.1056/NEJMoa052933. [DOI] [PubMed] [Google Scholar]
- Fidler IJ. The pathogenesis of cancer metastasis: the 'seed and soil' hypothesis revisited. Nat Rev Cancer. 2003;3:453–458. doi: 10.1038/nrc1098. [DOI] [PubMed] [Google Scholar]
- Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H, Chen H, Omeroglu G, Meterissian S, Omeroglu A, et al. Stromal gene expression predicts clinical outcome in breast cancer. Nat Med. 2008;14:518–527. doi: 10.1038/nm1764. [DOI] [PubMed] [Google Scholar]
- Friedl P, Wolf K. Tumour-cell invasion and migration: diversity and escape mechanisms. Nat Rev Cancer. 2003;3:362–374. doi: 10.1038/nrc1075. [DOI] [PubMed] [Google Scholar]
- Giampieri S, Manning C, Hooper S, Jones L, Hill CS, Sahai E. Localized and reversible TGFβ signaling switches breast cancer cells from cohesive to single cell motility. Nat Cell Biol. 2009;11:1287–1296. doi: 10.1038/ncb1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert LA, Hemann MT. DNA damage-mediated induction of a chemoresistant niche. Cell. 2010;143:355–366. doi: 10.1016/j.cell.2010.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gocheva V, Wang HW, Gadea BB, Shree T, Hunter KE, Garfall AL, Berman T, Joyce JA. IL-4 induces cathepsin protease activity in tumor-associated macrophages to promote cancer growth and invasion. Genes Dev. 2010;24:241–255. doi: 10.1101/gad.1874010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetz JG, Minguet S, Navarro-Lérida I, Lazcano JJ, Samaniego R, Calvo E, Tello M, Osteso-Ibáñez T, Pellinen T, Echarri A, et al. Biochemical remodeling of the microenvironment by stromal caveolin-1 favors tumor invasion and metastasis. Cell. 2011;146:148–163. doi: 10.1016/j.cell.2011.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grivennikov SI, Greton FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo W, Giancotti FG. Integrin signalling during tumour progression. Nat Rev Mol Cell Biol. 2004;5:816–826. doi: 10.1038/nrm1490. [DOI] [PubMed] [Google Scholar]
- Gupta GP, Massagué J. Cancer metastasis: building a framework. Cell. 2006;127:679–695. doi: 10.1016/j.cell.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Gupta GP, Nguyen DX, Chiang AC, Bos PD, Kim JY, Nadal C, Gomis RR, Manova-Todorova K, Massagué J. Mediators of vascular remodelling co-opted for sequential steps in lung metastasis. Nature. 2007a;446:765–770. doi: 10.1038/nature05760. [DOI] [PubMed] [Google Scholar]
- Gupta GP, Perk J, Acharyya S, de Candia P, Mittal V, Todorova-Manova K, Gerald WL, Brogi E, Benezra R, Massagué J. ID genes mediate tumor reinitiation during breast cancer lung metastasis. Proc Natl Acad Sci USA. 2007b;104:19506–19511. doi: 10.1073/pnas.0709185104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta RA, Shah N, Wang KC, Kim J, Horlings HM, Wong DJ, Tasi M, Hung T, Argani P, Rinn JL, et al. Long non-coding RNA HOTAIR reprograms chromatin state to promote cancer metastasis. Nature. 2010;464:1071–1076. doi: 10.1038/nature08975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart IR, Fidler IJ. Role of organ selectivity in the determination of metastatic patterns of the B16 melanoma. Cancer Res. 1980;40:2281–2287. [PubMed] [Google Scholar]
- Hiratsuka S, Duda DG, Huang Y, Goel S, Sugiyama T, Nagasawa T, Fukumura D, Jain RK. C-X-C receptor type 4 promotes metastasis by activating p38 mitogen-activated protein kinase in myeloid differentiation antigen (Gr-1)-positive cells. Proc Natl Acad Sci USA. 2011a;108:302–307. doi: 10.1073/pnas.1016917108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiratsuka S, Goel S, Kamoun WS, Maru Y, Fukumura D, Duda DG, Jain RK. Endothelial focal adhesion kinase mediates cancer cell homing to discrete regions of the lungs via E-selectin upregulation. Proc Natl Acad Sci USA. 2011b;108:3725–3730. doi: 10.1073/pnas.1100446108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland SJ, Pan A, Franci C, Hu Y, Chang B, Li W, Duan M, Tonreros A, Yu J, Heckrodt TJ, et al. R428, a selective small molecule inhibitor of Axl kinase, blocks tumor spread and prolongs survival in models of metastatic breast cancer. Cancer Res. 2010;70:1544–1554. doi: 10.1158/0008-5472.CAN-09-2997. [DOI] [PubMed] [Google Scholar]
- Hu M, Yao J, Carroll DK, Weremowicz S, Chen H, Carrasco D, Richardson A, Violette S, Nikolskaya T, Nikolsky Y, et al. Regulation of in situ to invasive breast carcinoma transition. Cancer Cell. 2008;13:394–406. doi: 10.1016/j.ccr.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Song N, Ding Y, Yuan S, Li X, Cai H, Shi H, Luo Y. Pulmonary vascular destabilization in the premetastatic phase facilitates lung metastasis. Cancer Res. 2009;69:7529–7537. doi: 10.1158/0008-5472.CAN-08-4382. [DOI] [PubMed] [Google Scholar]
- Hüsemann Y, Geigl JB, Schubert F, Musiani P, Meyer M, Burghart E, Fomi G, Eils R, Fehm T, Riethmüller G, et al. Systemic spread is an early step in breast cancer. Cancer Cell. 2008;13:58–68. doi: 10.1016/j.ccr.2007.12.003. [DOI] [PubMed] [Google Scholar]
- Iwanicki MP, Davidowitz RA, Ng MR, Besser A, Muranen T, Merritt M, Danuser G, Ince T, Brugge JS. Ovarian cancer spheroids use myosin-generated force to clear the mesothelium. Cancer Discov. 2011;1:144–157. doi: 10.1158/2159-8274.CD-11-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S, Chen WD, Parmigiani G, Diehl F, Beerenwinkel N, Antal T, Traulsen A, Nowak MA, Siegel C, Velculescu VE, et al. Comparative lesion sequencing provides insights into tumor evolution. Proc Natl Acad Sci USA. 2008;105:4283–4288. doi: 10.1073/pnas.0712345105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce JA, Pollard JW. Microenvironmental regulation of metastasis. Nat Rev Cancer. 2009;9:239–252. doi: 10.1038/nrc2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang SY, Halvorsen OJ, Gravdal K, Bhattacharya N, Lee JM, Liu NW, Johnston BT, Johnston AB, Haukaas SA, Aamodt K, et al. Prosaposin inhibits tumor metastasis via paracrine and endocrine stimulation of stromal p53 and Tsp-1. Proc Natl Acad Sci USA. 2009;106:12115–12120. doi: 10.1073/pnas.0903120106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y, Siegel PM, Shu W, Drobnjak M, Kakonen SM, Cordón-Cardo C, Guise TA, Massagué J. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell. 2003;3:537–549. doi: 10.1016/s1535-6108(03)00132-6. [DOI] [PubMed] [Google Scholar]
- Kessenbrock K, Plaks V, Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell. 2010;141:52–67. doi: 10.1016/j.cell.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M, Oskarsson T, Acharyya S, Nguyen DX, Zhang XH, Norton L, Massagué J. Tumor self-seeding by circulating cancer cells. Cell. 2009;139:1315–1326. doi: 10.1016/j.cell.2009.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein CA. Parallel progression of primary tumours and metastases. Nat Rev Cancer. 2009;9:302–312. doi: 10.1038/nrc2627. [DOI] [PubMed] [Google Scholar]
- Kouros-Mehr H, Bechis SK, Slorach EM, Littlepage LE, Egeblad M, Ewald AJ, Pai SY, Ho IC, Werb Z. GATA-3 links tumor differentiation and dissemination in a luminal breast cancer model. Cancer Cell. 2008;13:141–152. doi: 10.1016/j.ccr.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, Fong SF, Csiszar K, Giaccia A, Weninger W, et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139:891–906. doi: 10.1016/j.cell.2009.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W, Laitinen S, Khan S, Vihinen M, Kowalski J, Yu G, Chen L, Ewing CM, Eisenberger MA, Carducci MA, et al. Copy number analysis indicated monoclonal origin of lethal metastatic prostate cancer. Nat Med. 2009;15:559–565. doi: 10.1038/nm.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu J, Getz G, Miska EA, Alvarez-Saavedra E, Lamb J, Peck D, Sweet-Cordero A, Ebert BL, Mak RH, Ferrando AA, et al. MicroRNA expression profiles classify human cancers. Nature. 2005;435:834–838. doi: 10.1038/nature03702. [DOI] [PubMed] [Google Scholar]
- Luzzi KJ, MacDonald IC, Schmidt EE, Kerkvliet N, Morris VL, Chambers AF, Groom AC. Multistep nature of metastatic inefficiency: dormancy of solitary cells after successful extravasation and limited survival of early micrometastases. Am J Pathol. 1998;153:865–873. doi: 10.1016/S0002-9440(10)65628-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L, Reinhardt F, Pan E, Soutschek J, Bhat B, Marcusson EG, Teruya-Feldstein J, Bell GW, Weinberg RA. Therapeutic silencing of miR-10b inhibits metastasis in a mouse mammary tumor model. Nat Biotechnol. 2010;28:341–347. doi: 10.1038/nbt.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzieri R, Pucci F, Moi D, Zonari E, Ranghetti A, Berti A, Politi LS, Gentner B, Brown JL, Naldini L, et al. Targeting the ANG2/TIE2 axis inhibits tumor growth and metastasis by impairing angiogenesis and disabling rebounds of proangiogenic myeloid cells. Cancer Cell. 2011;19:512–526. doi: 10.1016/j.ccr.2011.02.005. [DOI] [PubMed] [Google Scholar]
- McAllister SS, Gifford AM, Greiner AL, Kelleher SP, Saelzler MP, Ince TA, Reinhardt F, Harris LN, Hylander BL, Repasky EA, et al. Systemic endocrine instigation of indolent tumor growth requires osteopontin. Cell. 2008;133:994–1005. doi: 10.1016/j.cell.2008.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng S, Tripathy D, Frenkel EP, Shete S, Naftalis EZ, Huth JF, Beitsch PD, Leitch M, Hoover S, Euhus D, et al. Circulating tumor cells in patients with breast cancer dormancy. Clin Cancer Res. 2004;10:8152–8162. doi: 10.1158/1078-0432.CCR-04-1110. [DOI] [PubMed] [Google Scholar]
- Miles D, Harbeck N, Escudier B, Hurwitz H, Saltz L, Van Cutsem E, Cassidy J, Mueller B, Sirzén F. Disease course patterns after discontinuation of bevacizumab: pooled analysis of randomized phase III trials. J Clin Oncol. 2011;29:83–88. doi: 10.1200/JCO.2010.30.2794. [DOI] [PubMed] [Google Scholar]
- Minn AJ, Gupta GP, Siegel PM, Bos PD, Shu W, Giri DD, Viale A, Olshen AB, Gerald WL, Massagué J. Genes that mediate breast cancer metastasis to lung. Nature. 2005;436:518–524. doi: 10.1038/nature03799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagrath S, Sequist LV, Maheswaran S, Bell DW, Irimia D, Ulkus L, Smith MR, Kwak EL, Digumarthy S, Muzikansky A, et al. Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature. 2007;450:1235–1239. doi: 10.1038/nature06385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navin N, Kendall J, Troge J, Andrews P, Rodgers L, McIndoo J, Cook K, Stepansky A, Levy D, Esposito D, et al. Tumour evolution inferred by single-cell sequencing. Nature. 2011;472:90–94. doi: 10.1038/nature09807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen DX, Bos PD, Massagué J. Metastasis: from dissemination to organ-specific colonization. Nat Rev Cancer. 2009;9:274–284. doi: 10.1038/nrc2622. [DOI] [PubMed] [Google Scholar]
- Olive KP, Jacobetz MA, Davidson CJ, Gopinathan A, McIntyre D, Honess D, Madhu B, Golgraben MA, Caldwell ME, Allard D, et al. Inhibition of Hedgehog singaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science. 2009;324:1457–1461. doi: 10.1126/science.1171362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oskarsson T, Acharyya S, Zhang XHF, Vanharanta S, Tavazoie SF, Morris PG, Downey RJ, Manova-Todorova K, Brogi E, Massagué J. Breast cancer cells produce tenascin C as a metastatic niche component to colonize the lungs. Nat Med. 2011;17:867–874. doi: 10.1038/nm.2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oskarsson T, Nagorny P, Krauss IJ, Perez L, Mandal M, Yang G, Ouerfelli O, Xiao D, Moore MA, Massagué J, et al. Diverted total synthesis leads to the generation of promising cell-migration inhibitors for treatment of tumor metastasis: in vivo and mechanistic studies on the migrastatin core ether analog. J Am Chem Soc. 2010;132:3224–3228. doi: 10.1021/ja9101503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padera TP, Kuo AH, Hoshida T, Laio S, Lobo J, Kozak KR, Fukumura D, Jain RK. Differential response of primary tumor versus lymphatic metastasis to VEGFR-2 and VEGFR-3 kinase inhibitors cediranib and vandetanib. Mol Cancer Ther. 2008;7:2272–2279. doi: 10.1158/1535-7163.MCT-08-0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padua D, Zhang XH, Wang Q, Nadal C, Gerald WL, Gomis RR, Massagué J. TGFbeta primes breast tumors for lung metastasis seeding through angiopoietin-like 4. Cell. 2008;133:66–77. doi: 10.1016/j.cell.2008.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Páez-Ribes M, Allen E, Hudock J, Takeda T, Okuyama H, Viñals F, Inoue M, Bergers G, Hanahan D, et al. Antiangiogenic therapy elicits malignant progression of tumors to increased local invasion and distant metastasis. Cancer Cell. 2009;15:220–231. doi: 10.1016/j.ccr.2009.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–2826. doi: 10.1056/NEJMoa041588. [DOI] [PubMed] [Google Scholar]
- Palmeiri D, Halverson DO, Ouatas T, Horak CE, Salerno M, Johnson J, Figg WD, Hollingshead M, Hursting S, Berrigan D, et al. Medroxyprogesterone acetate elevation of Nm23-H1 metastasis suppressor expression in hormone receptor-negative breast cancer. J Natl Cancer Inst. 2005;97:632–642. doi: 10.1093/jnci/dji111. [DOI] [PubMed] [Google Scholar]
- Pantel K, Brakenhoff RH, Brandt B. Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nat Rev Cancer. 2008;8:329–340. doi: 10.1038/nrc2375. [DOI] [PubMed] [Google Scholar]
- Podsypanina K, Du YC, Jechlinger M, Beverly LJ, Hambardzumvan D, Varmus H. Seeding and propagation of untransformed mouse mammary cells in the lung. Science. 2008;321:1841–1844. doi: 10.1126/science.1161621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psaila B, Lyden D. The metastatic niche: adapting the foreign soil. Nat Rev Cancer. 2009;9:285–293. doi: 10.1038/nrc2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian B, Li J, Zhang H, Kitamura T, Zhang J, Campion LR, Kaiser EA, Snyder LA, Pollard JW. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011;475:222–225. doi: 10.1038/nature10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian B, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaswamy S, Ross KN, Lander ES, Golub TR. A molecular signature of metastasis in primary solid tumors. Nat Genet. 2003;33:49–54. doi: 10.1038/ng1060. [DOI] [PubMed] [Google Scholar]
- Ricci-Vitiani L, Pallini R, Biffoni M, Todaro M, Invernici G, Cenci T, Maira G, Parati EA, Stassi G, Larocca LM, et al. Tumour vascularization via endothelial differentiation of glioblastoma stem-like cells. Nature. 2010;468:824–828. doi: 10.1038/nature09557. [DOI] [PubMed] [Google Scholar]
- Sahai E. Illuminating the metastatic process. Nat Rev Cancer. 2007;7:737–749. doi: 10.1038/nrc2229. [DOI] [PubMed] [Google Scholar]
- Schafer ZT, Grassian AR, Song L, Jiang Z, Gerhart-Hines Z, Irie HY, Gao S, Puigserver P, Brugge JS. Antioxidant and oncogene rescue of metabolic defects caused by loss of matrix attachment. Nature. 2009;461:109–113. doi: 10.1038/nature08268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt-Kittler O, Ragg T, Daskalakis A, Granzow M, Ahr A, Blankenstein TJ, Kaufmann M, Diebold J, Arnholdt H, Muller P, et al. From latent disseminated cells to overt metastasis: genetic analysis of systemic breast cancer progression. Proc Natl Acad Sci USA. 2003;100:7737–7742. doi: 10.1073/pnas.1331931100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzenback H, Hoon DS, Pantel K. Cell-free nucleic acids as biomarkers in cancer patients. Nat Rev Cancer. 2011;11:426–437. doi: 10.1038/nrc3066. [DOI] [PubMed] [Google Scholar]
- Sethi N, Dai X, Winter CG, Kang Y. Tumor-derived jagged1 promotes osteolytic bone metastasis of breast cancer by engaging notch signaling in bone cells. Cancer Cell. 2011;19:192–205. doi: 10.1016/j.ccr.2010.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shackleton M, Quintana E, Fearon ER, Morrison SJ. Heterogeneity in cancer: cancer stem cells versus clonal evolution. Cell. 2009;138:822–829. doi: 10.1016/j.cell.2009.08.017. [DOI] [PubMed] [Google Scholar]
- Shibue T, Weinberg RA. Integrin beta1-focal adhesion kinase signaling directs the proliferation of metastatic cancer cells disseminated in the lungs. Proc Natl Acad Sci USA. 2009;106:10290–10295. doi: 10.1073/pnas.0904227106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimono Y, Zabala M, Cho RW, Lobo N, Dalerba P, Qian D, Diehn M, Liu H, Panula SP, Chiao E, et al. Downregulation of miRNA-200c links breast cancer stem cells with normal stem cells. Cell. 2009;138:592–603. doi: 10.1016/j.cell.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonoshita M, Aoki M, Fuwa H, Aoki K, Hosogi H, Sakai Y, Hashida H, Takabayashi A, Sasaki M, Robine S, et al. Suppression of colon cancer metastasis by Aes through inhibition of Notch signaling. Cancer Cell. 2011;19:125–137. doi: 10.1016/j.ccr.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Steeg PS. Tumor metastasis: mechanistic insights and clinical challenges. Nat Med. 2006;12:895–904. doi: 10.1038/nm1469. [DOI] [PubMed] [Google Scholar]
- Stott SL, Hsu CH, Tsukrov DI, Yu M, Miyamoto DT, Waltman BA, Rothenberg SM, Shah AM, Smas ME, Korir GK, et al. Isolation of circulating tumor cells using a microvortex-generating herringbone-chip. Proc Natl Acad Sci USA. 2010;107:18392–18397. doi: 10.1073/pnas.1012539107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratton MR. Exploring the genomes of cancer cells: progress and promise. Science. 2011;331:1553–1558. doi: 10.1126/science.1204040. [DOI] [PubMed] [Google Scholar]
- Tabariès S, Dong Z, Annis MG, Omeroglu A, Pepin F, Ouellet V, Russo C, Hassanain M, Metrakos P, Diaz Z, et al. Claudin-2 is selectively enriched in and promotes the formation of breast cancer liver metastases through engagement of integrin complexes. Oncogene. 2011;30:1318–1328. doi: 10.1038/onc.2010.518. [DOI] [PubMed] [Google Scholar]
- Tarin D, Price JE, Kettlewell MG, Souter RG, Vass AC, Crossley B. Mechanisms of human tumor metastasis studied in patients with peritoneovenous shunts. Cancer Res. 1984;44:3584–3592. [PubMed] [Google Scholar]
- Thiery JP, Acloque H, Huang RYJ, Neito MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Valastyan S, Chang A, Benaich N, Reinhardt F, Weinberg RA. Activation of miR-31 function in already-established metastases elicits metastatic regression. Genes Dev. 2011;25:646–659. doi: 10.1101/gad.2004211. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Valastyan S, Reinhardt F, Benaich N, Calogrias D, Szász AM, Wang ZC, Brock JE, Richardson AL, Weinberg RA. A pleiotropically acting microRNA, miR-31, inhibits breast cancer metastasis. Cell. 2009;137:1032–1046. doi: 10.1016/j.cell.2009.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Valastyan S, Weinberg RA. MicroRNAs: crucial multi-tasking components in the complex circuitry of tumor metastasis. Cell Cycle. 2009;8:3506–3512. doi: 10.4161/cc.8.21.9802. [DOI] [PubMed] [Google Scholar]
- van’t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Mao M, Peterse HL, van der Kooy K, Marton MJ, Witteveen AT, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415:530–536. doi: 10.1038/415530a. [DOI] [PubMed] [Google Scholar]
- Wang R, Chadalavada K, Wilshire J, Kowalik U, Hovinga KE, Geber A, Fligelman B, Leversha M, Brennan C, Tabar V. Glioblastoma stem-like cells give rise to tumour endothelium. Nature. 2010;468:829–833. doi: 10.1038/nature09624. [DOI] [PubMed] [Google Scholar]
- Wang W, Goswami S, Lapidus K, Wells AL, Wyckoff JB, Sahai E, Singer RH, Segall JE, Condeelis JS. Identification and testing of a gene expression signature of invasive carcinoma cells within primary mammary tumors. Cancer Res. 2004;64:8585–8594. doi: 10.1158/0008-5472.CAN-04-1136. [DOI] [PubMed] [Google Scholar]
- Weigelt B, Glas AM, Wessels LF, Witteveen AT, Peterse JL, van’t Veer LJ. Gene expression profiles of primary breast tumors maintained in distant metastases. Proc Natl Acad Sci USA. 2003;100:15901–15905. doi: 10.1073/pnas.2634067100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weilbaecher KN, Guise TA, McCauley LK. Cancer to bone: a fatal attraction. Nat Rev Cancer. 2011;11:411–425. doi: 10.1038/nrc3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weis S, Cui J, Barnes L, Cheresh Endothelial barrier disruption by VEGF-mediated Src activity potentiates tumor cell extravasation and metastasis. J Cell Biol. 2004;167:223–229. doi: 10.1083/jcb.200408130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winslow MM, Dayton TL, Verhaak RGW, Kim-Kiselak C, Snyder EL, Feldser DM, Hubbard DD, DuPage MJ, Whittaker CA, Hoersch S, et al. Suppression of lung adenocarcinoma progression by Nkx2-1. Nature. 2011;473:101–104. doi: 10.1038/nature09881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyckoff JB, Wang Y, Lin EY, Li JF, Goswami S, Stanley ER, Segall JE, Pollard JW, Condeelis J. Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors. Cancer Res. 2007;67:2649–2656. doi: 10.1158/0008-5472.CAN-06-1823. [DOI] [PubMed] [Google Scholar]
- Yachida S, Jones S, Bozic I, Antal T, Leary R, Fu B, Kamiyama M, Hruban RH, Eshleman JR, Nowak MA, et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature. 2010;467:1114–1117. doi: 10.1038/nature09515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu SL, Chen HY, Chang GC, Chen CY, Singh S, Cheng CL, Yu CJ, Lee YC, Chen HS, Su TJ, et al. MicroRNA signature predicts survival and relapse in lung cancer. Cancer Cell. 2008;13:48–57. doi: 10.1016/j.ccr.2007.12.008. [DOI] [PubMed] [Google Scholar]
- Zhang XH, Wang Q, Gerald W, Hudis CA, Norton L, Smid M, Foekens JA, Massagué J. Latent bone metastasis in breast cancer tied to Src-dependent survival signals. Cancer Cell. 2009;16:67–78. doi: 10.1016/j.ccr.2009.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]