Protein O-linked ß-N-acetylglucosamine: A novel effector of cardiomyocyte metabolism and function (original) (raw)
. Author manuscript; available in PMC: 2014 Feb 19.
Published in final edited form as: J Mol Cell Cardiol. 2011 Aug 22;52(3):538–549. doi: 10.1016/j.yjmcc.2011.08.009
Abstract
The post-translational modification of serine and threonine residues of nuclear and cytoplasmic proteins by the O-linked attachment of the monosaccharide ß-N-acetyl-glucosamine (O-GlcNAc) is emerging as an important mechanism for the regulation of numerous biological processes critical for normal cell function. Active synthesis of O-GlcNAc is essential for cell viability and acute activation of pathways resulting in increased protein O-GlcNAc levels improves the tolerance of cells to a wide range of stress stimuli. Conversely sustained increases in O-GlcNAc levels have been implicated in numerous chronic disease states, especially as a pathogenic contributor to diabetic complications. There has been increasing interest in the role of O-GlcNAc in the heart and vascular system and acute activation of O-GlcNAc levels have been shown to reduce ischemia/reperfusion injury attenuate vascular injury responses as well mediate some of the detrimental effects of diabetes and hypertension on cardiac and vascular function. Here we provide an overview of our current understanding of pathways regulating protein O-GlcNAcylation, summarize the different methodologies for identifying and characterizing O-GlcNAcylated proteins and subsequently focus on two emerging areas: 1) the role of O-GlcNAc as a potential regulator of cardiac metabolism and 2) the cross talk between O-GlcNAc and reactive oxygen species.
Introduction
Classical protein glycosylation involves the synthesis of complex elongated oligosaccharide structures via N-linkage on asparagine and O-linkage on the hydroxy amino acids serine (Ser) and threonine (Thr), as well as hydroxyproline, hydroxylysine, and tyrosine residues of proteins that become secreted or membrane component glycoproteins [1]. Importantly these glycosylation reactions occur exclusively in the ER and Golgi; however, in 1984 a novel glycosylation modification was first reported in which a single ß-N-acetyl-glucosamine moiety was attached via a O-linkage to serine (Ser) and threonine (Thr) residues of cytoplasmic and nuclear proteins [2]. This modification, now commonly known as O-GlcNAc, has been shown to be present on over 1000 nuclear, cytoplasmic and mitochondrial proteins and has been found in all metazoans, as well as in some bacteria, protozoa, viruses and fungi [3-7]. O-GlcNAcylation is distinct from traditional glycosylation in that it is restricted to the cytoplasm, nucleus and mitochondria, it is not extended into complex elongated structures; it also exhibits parallels with protein phosphorylation, in that it responds to acute stimuli, alters protein function and enzyme activity and modifies the same or proximal Ser/Thr residues as phosphorylation [3-7].
It has become increasingly apparent that O-GlcNAc modification of proteins is an important mechanism for the regulation of numerous biological processes critical for normal cell function such as signal transduction [8-11], proteasome activity [12, 13], apoptosis [14, 15], nuclear transport [16], translation and transcription [17]. Most of our understanding of the impact of alterations in O-GlcNAc levels on cell function has come from studies of chronic disease models such as cancer [18-20], senescence [21-23], neurodegeneration [11, 14, 24, 25] as well as diabetes and diabetic complications [26, 27]. However, a number of studies have demonstrated that O-GlcNAc is essential for cell viability [28-30] and that acute activation of pathways resulting in increased protein O-GlcNAc levels improves the tolerance of cells to a wide range of stress stimuli [29].
There has been increasing interest in the role of O-GlcNAc in the heart and vascular system and acute activation of O-GlcNAc levels has been shown to reduce ischemia/reperfusion injury [31-41], attenuate vascular injury responses [42] as well mediate some of the detrimental effects of diabetes [21, 43-49] and hypertension [50-53] on cardiac and vascular function. The growing awareness of the effects of altered O-GlcNAc on cardiovascular function is reflected in part by a relatively large number of reviews on this subject over the past few years [37, 52-58]. Therefore, in light of these and other recent comprehensive reviews on O-GlcNAc biology [3-7], we provide an brief summary on the regulation of O-GlcNAc synthesis, followed by practical overview regarding the 1) modulation of cellar O-GlcNAc levels and 2) the characterization and identification of O-GlcNAcylated proteins. We then focus on two emerging areas, namely the role of O-GlcNAc as a potential regulator of cardiac metabolism and the cross talk between O-GlcNAc and reactive oxygen species, with an emphasis on the role of mitochondria in mediating this interaction.
Regulation of O-GlcNAc synthesis and turnover
The primary components involved in regulating O-GlcNAc synthesis and turnover are summarized in Fig 1. Uridine-diphosphate-N-acetylglucosamine (UDP-GlcNAc) is the sugar nucleotide donor for the synthesis of O-GlcNAc modified proteins, by O-GlcNAc transferase (OGT). OGT has a high affinity for UDP-GlcNAc, which provides it with a competitive advantage over nucleotide transporters in the endoplasmic reticulum and Golgi that compete for cytoplasmic UDP-GlcNAc, but also makes it highly sensitive to changes in UDP-GlcNAc concentrations [59]. Thus, the rate of O-GlcNAc synthesis and overall levels of O-GlcNAc protein modification are highly dependent on the flux through hexosamine biosynthesis pathway (HBP). HBP flux is regulated largely by L-glutamine-d-fructose 6-phosphate amidotransferase (GFAT), which converts fructose-6-phosphate to glucosamine-6-phosphate with glutamine as the amine donor [60].
Figure 1. The hexosamine biosynthesis pathway (HBP) and protein O-GlcNAcylation.
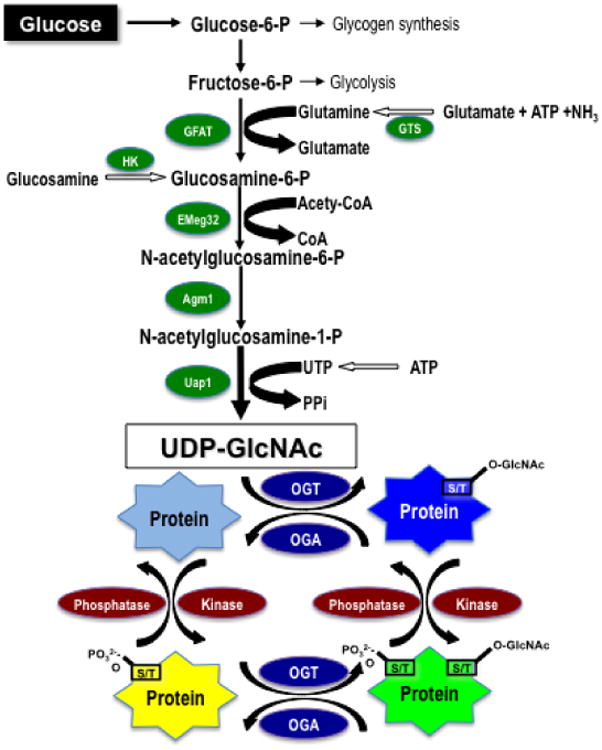
Glucose imported into the cells is rapidly phosphorylated to glucose-6-phosphate and converted to fructose-6-phosphate, which is subsequently metabolized to glucosamine-6-phosphate by L-glutamine-D-fructose 6-phosphate amidotransferase (GFAT). Synthesis of glucosamine-6-phosphate is dependent on availability of glutamine, which is formed by glutamine synthetase (GTS). Glucosamine-6-phosphate is subsequently metabolized by glucosamine 6-phosphate N-acetyltransferase (Emeg32) to N-acetylglucosamine-6-phosphate, which is converted to N-acetylglucosamine-1-phosphate by Phosphoacetylglucosamine mutase (Agm1) and the synthesis of UDP- uridine-diphosphate-N-acetylglucosamine (UDP-GlcNAc) is catalyzed by UDP-N-acetylglucosamine pyrophosphorylase (Uap1). Flux through the HBP can be increased with glucosamine, which is phosphorylated by hexokinase (HK) to form glucosamine 6-phosphate thereby bypassing GFAT. UDP-GlcNAc is the obligatory substrate for OGT (uridine-diphospho-N-acetylglucosamine: polypeptide β-N-acetylglucosaminyltransferase) leading to the formation of O-linked ß-N-acetylglucosamine (O-GlcNAc)-modified proteins. ß-N-acetylglucosaminidase (OGA) catalyzes the removal of O-GlcNAc from the proteins.
Cell culture studies suggest that ∼2–5% of total glucose entering the cell is metabolized via GFAT [61]; however, the extent to which this holds true for a highly metabolic organ, such as the heart is unknown. GFAT is considered to be the primary rate-determining step in the HBP and exists in two isoforms (GFAT1 and GFAT2), transcribed from separate genes. In the heart GFAT2 is the most abundant isoform [62] and in rodent models of aging [23] and pressure overload hypertrophy [63] there were significant increases in GFAT2 mRNA levels, but little or no change in GFAT1 mRNA levels. In both studies there were also increased UDP-GlcNAc levels, consistent with an increase in HBP flux, suggesting that GFAT expression and HBP flux in the heart are subject to regulation in response to chronic stress. It is also of note that both GFAT1 and GFAT2 are subject to phosphorylation by cAMP-dependent protein kinase [64, 65]; in addition both AMPK and CaMKII lead to phosphorylation of Se243 of human GFAT1 resulting in increased enzyme activity [66]. While the our understanding of the regulation of GFAT activity remains poorly understood, the fact that it appears to be a target for AMPK, raises the possibility that it is a key link between AMPK, the HBP and O-GlcNAc signaling (Fig 2).
Figure 2. Acute and transcriptional regulation of cardiac metabolism mediated by the hexosamine biosynthesis pathway (HBP) and O-GlcNAc.
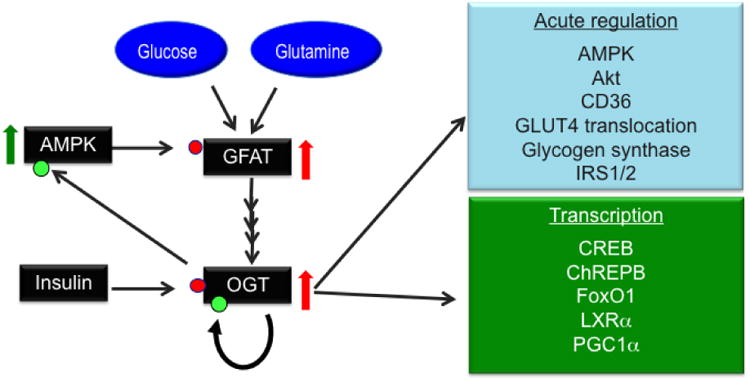
Flux through the HBP is regulated by glutamine-D-fructose 6-phosphate amidotransferase (GFAT) and is dependent on the availability of glucose and glutamine. O-GlcNAc transferase (OGT) is subject to both O-GlcNAcylation (green circles) and insulin-mediated phosphorylation (red circles) both of which have been reported to increase its activity. AMPK, which is well recognized as a key regulator of cellular metabolism has been reported to be a target for O-GlcNAcylation and that this increases its activity; furthermore, GFAT has been shown to phosphorylated by AMPK also leading to increased activity. This provides a feed forward loop leading to further increase in OGT activity and subsequent increase in O-GlcNAcylation. Increases in O-GlcNAc levels can potentially acutely regulate cardiac metabolism, not only by modification of AMPK, but also by O-GlcNAcylation of other key mediators of carbohydrate and fatty acid metabolism. A number of transcription factors, which play critical role in the longer-term regulation of metabolism, are also known to be O-GlcNAcylated.
Following its synthesis by GFAT, glucosamine-6-phosphate is metabolized via glucosamine 6-phosphate N-acetyltransferase (Emeg32), phosphoacetylglucosamine mutase (Agm1) and finally UDP-N-acetylglucosamine pyrophosphorylase (Uap1) to UDP-GlcNAc (Fig 1). The HBP is often referred to as a “nutrient-sensing” pathway, and this highlighted by the fact that in addition to glucose availability, UDP-GlcNAc synthesis is dependent on amino acid metabolism, specifically the availability of glutamine; acetyl-CoA derived from either pyruvate or fatty acid metabolism as well as high energy phosphates in the form of ATP and UTP. Thus, the synthesis of UDP-GlcNAc is critically dependent on the coordinated action of several key metabolic pathways in addition to glucose. The importance of the HBP and UDP-GlcNAc synthesis for cell viability is also emphasized by the fact that gene deletion of either EMeg32 or Agm1 is embryonically lethal [67, 68]; surprisingly however, remarkably little is known about the regulation of HBP flux in the heart or indeed in other tissues.
In addition to being a substrate for traditional glycosylation, UDP-GlcNAc is also a substrate for OGT, a unique glycosyl transferase, which catalyzes the attachment of O-GlcNAc to specific Ser/Thr residues of nuclear and cytoplasmic proteins. In humans and mice there is a single OGT gene located on the X chromosome [69-71], which through alternative splicing leads to three isoforms: 1) nucleocytoplasmic, ncOGT, (100kDa); 2) short form, sOGT (78kDa) and 3) a mitochondrial form, mOGT (103kDa); each isoform has the same C-terminal catalytic domains, but different N-terminal domains contributing to different localization and targeting [69, 70, 72]. In muscle, kidney and liver, OGT exists as a heterotrimer consisting of two 110 kDa and one 78 kDa subunits [73]; in other tissues it is a homotrimer of three 110 kDa subunits [71]. The catalytic C-terminal domain is altered by tyrosine phosphorylation and is also a target for O-GlcNAcylation [71], suggesting a potential feedback regulatory element on OGT activity. Later we will discuss in more detail the fact that insulin increases both tyrosine phosphorylation and O-GlcNAcylation of OGT, leading to increased activity and transient translocation from nucleus to cytoplasm [74, 75]. The N-terminal domain of OGT contains multiple tetratricopeptide repeats (TPR), which mediate the protein-protein interactions involved in the recognition and activation of specific protein targets [59, 76].
The steady state level of protein O-GlcNAcylation is dependent on the rate of synthesis catalyzed by OGT as well as its rate of removal catalyzed by ß-N-acetylglucosaminidase (O-GlcNAcase) [77, 78]. As with OGT, O-GlcNAcase is highly conserved across species and is expressed in all tissues and unlike lysosomal hexosaminidases has a pH optimum in the neutral range, pH 4.5-6 [77, 78]. Also similar to OGT, O-GlcNAcase is also encoded by a single gene, with at least two alternative spliced isoforms [6]. The predominant splice variants are, a long >100kDa form, and a short form (∼70kDa) with the O-GlcNAcase catalytic regions in the N-terminal domain [6, 79]. The C-terminal region of the long isoform has a histone acetyltransferase like domain with a caspase cleavage site between the two regions suggesting potential regulation in response to apoptosis; however, cleavage per se does not appear affect the O-GlcNAcase activity, suggesting that this may have other regulatory roles, such as stabilization, localization or targeting [80-82]. The short form of O-GlcNAcase has a smaller C-terminal region and lacks the putative HAT domain found in the long form [6, 79]; little is known regarding the different functions or localization of these two O-GlcNAcase isoforms, although the long isoform appears to exhibit greater catalytic activity than the short isoform [79]. As with GFAT and OGT, our knowledge of the regulation of O-GlcNAcase activity remains limited; however, it is known to be both phosphorylated and modified by O-GlcNAc [78, 80].
Changes in cellular O-GlcNAc levels occur rapidly, with a response time of seconds to minutes in response to extracellular stimuli [83, 84], which not only distinguishes it from traditional forms of glycosylation, but also draws parallels with phosphorylation. Further similarities to phosphorylation are emphasized by the fact that O-GlcNAc also modifies Ser/Thr residues and in some cases phosphorylation and O-GlcNAcylation occur on the same residues. It is increasingly evident that there is a complex and extensive cross talk between O-GlcNAcylation and phosphorylation; for example, Wang et al., [85] reported that increasing overall cellular O-GlcNAc levels by inhibition of O-GlcNAcase decreased phosphorylation at 280 sites and increased phosphorylation at 148 sites. The potential for rapid cycling between O-GlcNAcylation and phosphorylation is further emphasized by the observations that OGT and O-GlcNAcase forms transient complexes with kinases and protein phosphatases [86, 87].
Pharmacological and Molecular Modulation of O-GlcNAc turnover
Experimentally O-GlcNAc levels can be increased by activating synthesis, which is commonly achieved by elevating extracellular glucose concentrations, adding extracellular glucosamine, or by preventing its removal by inhibiting O-GlcNAcase. Hyperglycemia (∼25mM glucose) increases overall O-GlcNAc levels in many cell lines including neonatal and adult cardiomyocytes [34, 45, 46]. While some of the effects of hyperglycemia in cardiomyocytes can be reversed by inhibition of GFAT with either 6-diazo-5-oxo-L-norleucine (DON) or O-diazoacetyl-L-serine (azaserine) [34, 46], hyperglycemia clearly has many other effects on cellular function other than increasing metabolism via the HBP. Additionally while azaserine and DON are commonly used as GFAT inhibitors, they are better characterized as amidotransferase inhibitors [88]; thus, conclusions based on their use should be made with caution. Glucosamine is readily transported by the glucose transporter systems, with a Km of 2-4mM for GLUT1 and GLUT4 [89], the primary glucose transporters in cardiomyocytes and subsequently phosphorylated by hexokinase to glucosamine 6-phosphate. Glucosamine 6-phosphate directly enters the HBP bypassing the key regulatory enzyme GFAT (Fig 1), resulting in an increase in UDP-GlcNAc and O-GlcNAc levels. In the perfused heart, 5mM glucosamine leads to 2 to 3 fold increase in O-GlcNAc levels within 15 mins [32] and as little as 100μM glucosamine has been shown to significantly augment O-GlcNAc levels in the heart [90]. Such studies highlight the dynamic nature of the HBP and O-GlcNAc synthesis in the heart; however, increasing UDP-GlcNAc levels can also impact the synthesis of other glycoconjugates [91, 92] and elevated levels of other intermediates in the HBP have the potential to alter other metabolic pathways such as glycogen synthesis [93]. Nevertheless, at the cellular level increasing OGT protein levels appears to have the same effects on cardiomyocytes as adding glucosamine [33, 94], suggesting that the predominant effect of glucosamine, at least in the short term, is to increase cellular O-GlcNAc levels. Several studies have reported that the addition of glucosamine results in depletion of ATP levels [95]; however, we have not observed any impact of glucosamine treatment on ATP levels in either cardiomyocytes or the intact perfused heart [34, 36, 90]. Furthermore, up to 10mM glucosamine also had no adverse effect on cardiac function [90].
PUGNAc [O-(2-acetamido-2-deoxy-d-glucopyranosylidene) amino-N-phenylcarbamate] is a widely used competitive inhibitor of O-GlcNAcase [96, 97] and by attenuating the removal of O-GlcNAc leads to significant increases in cellular O-GlcNAc levels in isolated cardiomyocytes, the isolated perfused heart and in vivo [31, 34, 38, 98]. Although a common tool for increasing O-GlcNAc levels PUGNAc is also equally effective as an inhibitor of lysosomal hexosaminidases [99], which raises concerns about is specificity. Recently two new classes of O-GlcNAcase inhibitors have been described; GlcNAcastatin [100] and NAG-thiazolines [99, 101], both of which exhibit several orders of magnitude greater specificity for O-GlcNAcase over other hexosaminidases and with Ki in vitro in the pico to nanomolar range. We have successfully used the NAG-thiazolines derivatives 1,2 dideoxy-2′-propyl-α-D-glycopyranoso-[2,1-d]-Δ2′-thiazoline (NAG-Bt) and 1,2 dideoxy-2′-ethylamino-α-D-glucopyranoso-[2,1-d]- Δ2′thiazoline (NAG-Ae) to increase O-GlcNAc levels in the perfused heart and cardiomyocytes [37]. In the perfused heart NAG-Bt had an EC50 of ∼30 μM for increasing overall O-GlcNAc levels [37]; in recent studies, in cardiomyocytes we found that NAG-Ae, also known as thiamet-G, had an EC50 of ∼100nM for increasing O-GlcNAc levels [102]. In addition to effectively increasing O-GlcNAc levels in isolated cardiomyocytes and hearts, preliminary studies in vivo demonstrate that i.p. administration of thiamet-G at a dose of 50mg/Kg resulted in a 2-3 fold increase in cardiac O-GlcNAc levels within 2 hrs of administration (Chatham data not shown). It is also worth noting that Yuzwa et al., [103] reported that thiamet-G added to drinking water was effective at increasing tissue O-GlcNAc levels; however, they did not report on the O-GlcNAc levels in the heart. We have observed no detrimental effects of O-GlcNAcase inhibitors on cardiac function in the perfused heart; thus, there appears to be no acute adverse effects of increasing cardiac O-GlcNAc levels by inhibiting O-GlcNAcase.
While it is possible to pharmacologically increase O-GlcNAc levels by either increasing synthesis or inhibiting degradation, there are limited options for decreasing O-GlcNAc levels. The most common approach has been to attenuate OGT protein levels at the cellular level either by using siRNA methods [33], increase O-GlcNAcase expression [40] or to delete OGT completely using Cre-lox technology [30]. In cell culture, OGT-null mouse embryonic fibroblasts (MEFs) grow normally up to 48 hrs, after which growth slows and cell death occurs around 4-5 days [30]. Watson et al., [104] reported the development of a cardiac specific, inducible OGT KO mouse and found that a reduction in OGT levels had no adverse effects under basal conditions, but did accelerate the development of contractile dysfunction in response to pressure overload. The lack of any effects of decreased OGT levels in the absence of additional stress was somewhat surprising, given that OGT gene deletion typically leads to cell death [30]. The reason for this lack of phenotype is unclear and could be linked to transduction mosaicism or incomplete penetrance, which can occur in such inducible models, or that while OGT levels are markedly lower, that there has been an adaptive response leading to decreased O-GlcNAcase protein, so that turnover rates of O-GlcNAc may not be significantly altered. Certainly in other cell systems deletion of OGT leads to a reduction in O-GlcNAcase protein, in what seems to be an attempt to maintain O-GlcNAc levels constant [30]. However, it is also possible that since cardiomyocytes are essentially terminally differentiated, that they are able to survive with very low levels of OGT until subject to additional stress.
The lack of high affinity specific inhibitors of OGT has represented a significant limitation in investigating the role of O-GlcNAc on cardiomyocyte function. Walker and colleagues identified potential OGT inhibitors, using an in vitro high throughput screening approaches [105]. These compounds were subsequently commercially available as OGT inhibitors (TimTec, LLC); however, while there have been some reports in cell-based systems demonstrating the effectiveness of these compounds in lowering O-GlcNAc levels [39, 106], they have not yet been fully validated as OGT inhibitors and thus should be used with caution. Indeed our experience with these compounds in decreasing O-GlcNAc levels cardiomyocytes has been unsuccessful and we found that in an isolated perfused heart model as little of 5μM of “TT04” resulted in a significant decline in cardiac function (Chatham, data not shown). Recently, Gloster et al. [107] described a novel sulphonated UDP-GlcNAc analog, which inhibited OGT in vitro with Ki of 8μM and significantly lowered O-GlcNAc levels in COS-7 cells. Clearly further studies are needed to better characterize such inhibitors, but if their specificity can be fully validated and any effects on other glycosylation reactions characterized, the availability of these or similar compounds could be a useful addition for the pharmacological modulation of cardiomyocyte O-GlcNAc turnover.
Identifying and characterizing O-GlcNAcylated proteins
Probing for Protein O-GlcNAc Modification with Antibodies, Enzymatic Labeling, and Metabolic Labeling
While it is increasingly appreciated that O-GlcNAcylation is an abundant PTM modification it has been very difficult to detect due to the low stoichiometry of modification with an estimated 5-10% occupancy at a particular site[108]; the fragile nature of the O-linkage during tandem mass spectrometric (MS/MS) sequencing, and the lack of tools available to study this modification. However, recent breakthroughs in enrichment strategies and mass spectrometric sequencing approaches have greatly facilitated the unambiguous identification of O-GlcNAc modified peptides. These techniques are revealing the ubiquitous and dynamic nature of this posttranslational modification and provide direct evidence that this previously overlooked modification provides an additional layer of posttranslational regulation of protein function.
Pan-specific anti-O-GlcNAc antibodies (CTD110.6, Pierce; RL2 Covance) have proven invaluable for monitoring changes in global protein O-GlcNAc modification by immunoblotting or for probing for the presence of the modification on a specific protein of interest. However, these antibodies vary greatly in their specificity and sensitivity toward different OGT substrates and thus recognize only a subset of O-GlcNAc modified proteins. To overcome this limitation, Teo et al. [109] have recently generated a suite of monoclonal anti-O-GlcNAc antibodies, now available from Millipore, which were combined for the immunoprecipitation of a more comprehensive pool of O-GlcNAc modified proteins. Identification of these proteins by mass spectrometry revealed over 200 candidate O-GlcNAc modified proteins [109]. These new antibodies represent much needed new tools that when coupled to MS/MS should facilitate the simultaneous identification of both the modified protein and the sites of modification.
Recent developments in chemoenzymatic techniques, where the O-GlcNAc moiety is enzymatically tagged with a chemically reactive handle, are enabling large-scale mass spectrometry-based proteomic analyses of O-GlcNAc modified proteins. The enzymatic transfer of [3H] galactose by β-1,4-galactosyltransferase (GalT), was originally utilized as sensitive and definitive alternative to western blotting with antibodies or HRP-conjugated lectins to confirm that a protein of interest possesses the O-GlcNAc modification [110]; however, the catalytic activity of GalT is now being exploited for chemoenzymatic tagging of GlcNAc using a genetically engineered GalT1 (Y298L) enzyme which accommodates larger chemically reactive analogs of UDP-galactose, UDP-N-azido-acetylgalactosamine (UDP-GalNAz) or UDP-keto-galactose [111]. Once the azido-sugar is incorporated it is reacted by azide-alkyne Huisgen cycloaddition (“click chemistry”) in the presence a copper catalyst with biotinylated or otherwise functionalized tags thereby enabling visualization and affinity purification [112]; specificity for O-GlcNAc is obtained by cleaving N-linked glycoproteins with PNGase F. This approach has been utilized to identify 32 putative O-GlcNAc modified proteins [113].
Cell membranes are permeable to per-O-acetylated N-azidoacetylglucosamine (Ac4GlcNAz), which once inside the cell is deacetylated to GlcNAz by intracellular esterases; this approach has been developed to incorporate chemically reactive sugars into O-GlcNAcylated proteins in intact cells. Initially endogenous enzymes in the GlcNAc salvage pathway were exploited to convert GlcNAz to UDP-GlcNAz and GlcNAz is then transferred to serine and threonine residues of substrate proteins by OGT. However, to overcome the low level of incorporation of GlcNAz into proteins, Bertozzi and coworkers have used N-azidoacetylgalactosamine (GalNAz) as a source of GlcNAz for metabolic labeling [114]; GalNAz can be converted to UDP-GlcNAz by UDP-galactose 4′-epimerase (GALE); following epimerization, UDP-GlcNAz is incorporated into O-GlcNAc modified proteins by OGT. This approach appears to be much more robust for the metabolic labeling of O-GlcNAc modified proteins [115]. The resulting azido sugar is then reacted with phosphine containing functionalized linkers for the enrichment and detection of GlcNAz containing proteins [116, 117]. Pratt and colleagues recently published a modification of the metabolic labeling strategy, where the GlcNAc analog contains a reactive alkyne (GlcNAlk) rather than an azide. The UDP-GlcNAlk is less susceptible to epimerization to the UDP-galactosamine analog and can be reacted by click chemistry with azide containing probes [118].
One drawback to chemoenzymatic and metabolic labeling is that the biotin-tagged O-GlcNAc modified peptide itself is rarely identified by tandem mass spectrometry. Therefore, these approaches typically yield a list of putative candidate proteins for which the presence and site(s) of O-GlcNAc modification must be confirmed in further studies; however, adaptations of the chemoenzymatic labeling strategy, which permit mapping the sites of O-GlcNAc modification are described below. A chemoenzymatic labeling approach has also been developed to monitor dynamic changes in the stoichiometry of O-GlcNAc modification on a protein of interest [119]. This involves labeling O-GlcNAc with a large tag that increases the molecular weight of the protein sufficiently to be resolved by SDS-PAGE. While this approach does not reveal the percent occupancy of O-GlcNAc modification at a particular amino acid, it offers a mechanism to screen for ligands or physiological conditions that influence the extent of mono-, di-, or tri- O-GlcNAc modification of a given protein. This approach provides an alternative to using site-specific anti-O-GlcNAc antibodies, high-resolution mass spectrometry, or radiolabels for the interrogation of crosstalk between O-GlcNAc and other posttranslational modifications.
Detection of the Sites of O-GlcNAc Modification by Tandem Mass Spectrometry (MS/MS)
The standard approach used to identify sites of posttranslational modification, is to digest the protein of interest using trypsin or other proteases. The resulting peptides are fragmented and peptide sequence and site(s) of modification can then be identified from the fragmentation pattern of the peptide by MS/MS. The O-GlcNAc modification, however, is not stable during conventional MS/MS approaches; upon collision with gas molecules, the GlcNAc moiety is lost from the Ser/Thr side chain prior to fragmentation of the peptide backbone precluding direct detection of the site of modification. Thus, O-GlcNAc as well as other fragile modifications go undetected during routine mass spectrometric analysis. The reproducible neutral loss of the monosaccharide from the peptide and/or generation of the GlcNAc oxonium ion (204.2 Da) may indicate the presence of an O-GlcNAc modified peptide and the mass spectrometer can be programmed to acquire additional data on peptides that exhibit this behavior [108]; nevertheless, the specific modification site cannot be identified.
Recent advances in alternative fragmentation approaches, electron capture dissociation (ECD) and electron transfer dissociation (ETD), permit sequencing of peptides with fragile modifications, such as O-GlcNAc [120]. The availability of ETD capability on commercially available ion trap and Orbitrap instruments and the continued development of algorithms for searching ETD MS/MS data against protein databases are enabling detection of this evasive modification [121, 122]. With a mass spectrometric method now available that allows direct identification of O-GlcNAc modified peptides and unambiguous determination of the site of modification, the remaining challenge is selectively enriching O-GlcNAc modified peptides from complex mixtures to overcome the limited dynamic range of the instrumentation.
Enrichment of O-GlcNAcylated Peptides for ETD MS/MS
To facilitate the identification of the sites of modification, O-GlcNAcylated peptides can be immunoprecipitated with pan-O-GlcNAc antibodies, enriched with wheat germ agglutinin (WGA) or succinylated WGA lectins, or affinity purified following chemoenzymatic labeling. The older O-GlcNAc antibodies, RL2 and CTD110.6, were of limited utility for immunoprecipitation due to either recognition of a limited number of proteins or relatively poor elution efficiency; however the newer antibodies appear to have improved properties for immunopurification of O-GlcNAcylated peptides and proteins [109].
During lectin weak affinity chromatography, a long WGA agarose column (> 3 m in length) is utilized to separate O-GlcNAc modified peptides from unmodified peptides [123, 124]. WGA lectin interacts predominately with the N-acetylhexosamines (HexNAc), N-acetylglucosamine (GlcNAc) and N-acetylgalactosamine (GalNAc). Highly glycosylated peptides are retained on the column while the migration of monosaccharide containing peptides is weakly retarded. Mass spectrometric analysis of the enriched mono-glycosylated peptides reveals the site of attachment at Asn or Ser/Thr but does not distinguish GlcNAc from GalNAc. The advantage of this approach is its simplicity and coupled with electron transfer dissociation MS/MS, the sites of O-linked HexNAc are directly identified without the need for enzymatic labeling or chemical derivatization. Recent studies have also coupled this enrichment approach to quantitative proteomic strategies to identify sites of O-GlcNAc modification that are dynamically regulated [125, 126].
Adaptations to the chemoenzymatic tagging approach, implemented specifically to enable mass spectrometric identification of biotin-tagged O-GlcNAc modified peptides, offer an alternative enrichment strategy that can be coupled to quantitative proteomic methodology. To overcome the difficulties in eluting biotinylated peptides from streptavidin beads and the inefficient backbone fragmentation of biotinylated peptides during MS/MS, peptides can be released from streptavidin beads by base catalyzed β-elimination [127] or by the use of a photocleavable biotinylated alkyne crosslinker [125]. One caveat of β-elimination is that this results in the release of peptides that no longer contain an O-GlcNAc tag, thus further studies must be performed to validate the site(s) of modification. In contrast, following photolysis the photocleavable linker leaves behind a tag that provides a signature fragmentation pattern by MS/MS and enables assignment of the site of modification. Although the chemoenzymatic tagging approach requires multiple sample preparation steps, advantages of this workflow include the ability to couple this approach to established quantitative proteomic procedures.
The use of isobaric tags (iTRAQ) or stable isotopic labeled amino acids in cell culture (SILAC) prior to enrichment of O-GlcNAcylated peptides permits the simultaneous identification of the site and relative quantitation of the extent of O-GlcNAc modification following a stimulus [126, 128, 129]. These studies require a high mass accuracy tandem mass spectrometer with the capability to fragment peptides by collision induced dissociation and electron transfer dissociation. The ability to couple quantitative proteomic approaches to the site-specific identification of O-GlcNAc modification will permit the unbiased discovery of the temporal dynamics and regulation of this modification during signal transduction. While alterations in the patterns of protein O-GlcNAc modification have been observed under varying physiological conditions in the heart, to date these proteins have not been identified. As sites of protein O-GlcNAc modification are published, they are made publically available in the Cell Signaling Phosphosite database [130] and dbOGAP [131]. The dbOGAP repository also contains information regarding known sites of phosphorylation that are in close proximity to the sites of O-GlcNAc modification. Large scale site-mapping experiments are revealing a loose consensus sequence and this information has being utilized to generate an algorithm for predicting sites of O-GlcNAc modification [131]. It has been estimated that with the emergence of these new MS and enrichment strategies, the total number of O-GlcNAc modification sites mapped over the past 2 years is greater than those identified during the past 20 years [3].
O-GlcNAcylation as a metabolic sensor and regulator
The HBP has long been recognized as a glucose-sensing pathway [6, 26, 132], but as noted earlier since it intersects with several key metabolic pathways it might be more accurately characterized as nutrient or metabolic sensing pathway. Increased flux through the HBP was first linked to the development of cellular insulin resistance in 1991 [61] and has been further supported by studies demonstrating that glucosamine infusion in vivo resulted in skeletal muscle insulin resistance [93, 133, 134] and also that GFAT overexpression in mice leads to insulin resistance [135, 136]. Glucosamine induced insulin resistance is also mediated by increased O-GlcNAcylation of IRS-1 and IRS-2 [134]. Increased cellular O-GlcNAc levels also decreased insulin stimulated GLUT4 translocation, reduced insulin-stimulated phosphorylation of IRS-1 and Akt as well as increased O-GlcNAc modifications of GLUT4, IRS-1 and Akt2 [137]. It is worth noting, however, that at the cellular level increased O-GlcNAcylation does not appear to be essential for the development of glucose/insulin-induced insulin resistance [138]. The syntaxin 4 binding protein, Munc18c is also modified by O-GlcNAc [139]; Munc18c contributes to membrane fusion events, involved in insulin-stimulated GLUT4 translocation and its modification by O-GlcNAc attenuated the response to insulin [139]. Chronic activation of the HBP also resulted in O-GlcNAcylation of AMPK, which was associated with increased activity and increased fatty acid oxidation [140]. Taken together, these data support the concept of O-GlcNAcylation as glucose sensing mechanism, and that elevated O-GlcNAc levels on several different key regulatory proteins, acts in a feed back manner to attenuate glucose entry. This is also consistent with the widely accepted notion that chronically elevated cellular O-GlcNAc levels is a contributing factor to the etiology of insulin resistance as well as a key mediator of glucose toxicity associated with the adverse effects of diabetes on numerous tissues including cardiomyocytes [5, 21, 27, 55]. It is of note that GFAT which regulates glucose flux into the HBP, is phosphorylated and activated by AMPK [66] and since O-GlcNAcylation is reported to increase AMPK activity, this could represent a feed forward mechanism, which if sustained may also contribute to O-GlcNAc mediated glucotoxicity (Fig 2).
While the studies highlighted above demonstrate a clear link between the HBP, O-GlcNAcylation levels and glucose metabolism it is striking that the focus is primarily on relatively long term regulation with an emphasis on the pathogenesis of insulin resistance and glucotoxicity. However, as noted above changes in O-GlcNAcylation can occur rapidly and we have demonstrated that relatively acute increases in O-GlcNAc levels can modulate the responses of cardiomyocytes and the intact heart to stress and agonist stimulation [32, 47, 83, 84]. This raises the question as to whether short term modulation of O-GlcNAc synthesis in the heart, could influence cardiac metabolism and substrate selection. To address this question, we recently examined the effects of glucosamine (0-10mM) on substrate utilization in the intact heart perfused with physiologically relevant concentrations of glucose, lactate, pyruvate, palmitate and insulin [90]. Perfusion for 60 min with as little as 50μM glucosamine significantly increased both UDP-GlcNAc and O-GlcNAc levels. While there are potential pathways for glucosamine metabolism, which could lead to an increase in glycolysis [141, 142], we found that glucosamine had no effect on either glucose oxidation or glycolytic flux [90]. Surprisingly, however, we found a significant increase in palmitate oxidation with a concomitant decrease in lactate and pyruvate oxidation reaching a maximal effect at 100μM glucosamine. In contrast to Luo et al., who reported that glucosamine stimulated fatty acid oxidation in cultured adipocytes was associated with increased AMPK and ACC phosphorylation [140], we observed no effect of glucosamine on either AMPK or ACC phosphorylation. On the other hand, membrane levels of FAT/CD36, which plays a key role in fatty acid transport in the heart, were significantly increased; furthermore, preliminary data suggested that FAT/CD36 is also a potential target for O-GlcNAcylation [90].
The spontaneously hypertensive rat (SHR), is a widely used genetic-model of hypertension, which expresses a different cd36 mRNA compared to Wistar controls rats and in the SHR heart, CD36 protein levels at plasma membrane are reduced [143]. Earlier studies by Des Rosiers and colleagues showed that the contribution of exogenous long-chain fatty acids to p-oxidation was significantly reduced in hearts from SHR rats [144] and they recently reported that this could be due to alterations in post-translational modifications of CD36 protein including changes in O-GlcNAc modification [145]. Consistent with our observations, they found that in hearts from control Wistar rats, 0.5mM glucosamine increased fatty acid oxidation >2 fold, but had no effect on fatty oxidation in hearts from SHRs, despite the fact that overall O-GlcNAc levels were increased to the same extent. They also reported that based on the predicted sequences for the wild-type and mutant CD36, the mutant CD36 had fewer potential sites for post-translational modification, including reduced O-GlcNAc modification sites. Further support for the HBP and by extension O-GlcNAc in regulating cardiac metabolism, was provided by the observation that glutamine, which is required for GFAT activity (Fig 1), also increases long-chain fatty acid metabolism and this can be reversed by inhibition of the HBP with azaserine [146]. Taken together these studies suggest a novel mechanism by which the HBP and O-GlcNAcylation could play a role in the acute regulation of cardiac metabolism. Specifically, these data have led us to postulate that an increase in glucose flux through the HBP, resulting in increased O-GlcNAcylation of CD36, leads to increased fatty acid transport and oxidation, which would have an indirect feed back effect on decreasing carbohydrate oxidation.
Young and colleagues have shown that in mice cardiac metabolism exhibits time of day dependent changes in both fatty acid and glucose metabolism which was associated with diurnal variations in total protein O-GlcNAcylation and abolished in hearts from cardiac clock mutant (CCM) mice [147]. Specifically they found that during the active phase there was increased myocardial protein O-GlcNAcylation suggesting increased flux of glucosyl moieties through the hexosamine biosynthetic pathway. Thus the cardiomyocyte circadian clock regulates nonoxidative fatty acid (i.e. triglyceride) and glucose (i.e. glycogen and O-GlcNAc) metabolism [148]. They also found that increased protein O-GlcNAcylation results in altered gene and protein expression of cardiomyocyte circadian clock components, as well as protein _O_-GlcNAcylation of CLOCK, raising the possibility that non-oxidative glucose metabolism is an integral component of the cardiomyocyte circadian clock, potentially mediated via proteins O-GlcNAcylation.
Yang et al., [74] provided further support for a close link between O-GlcNAc and metabolic regulation, by showing that insulin treatment leads to translocation of OGT from the nucleus to the plasma membrane, where it catalyzes the O-GlcNAcylation of key components of the insulin signaling pathway thereby attenuating insulin signal transduction. It was postulated that this represented one of the mechanisms contributing to O-GlcNAc mediated insulin resistance; however, these data also suggests a novel feedback loop, which could contribute to the short-term regulation of cellular metabolism. While further studies are clearly needed to demonstrate that HBP flux and O-GlcNAc turnover play a central and coordinated role in regulating cardiac metabolism it is clear that there is a close relationship between the HBP, O-GlcNAcylation and both acute regulation of myocardial substrate utilization as well as transcriptionally mediated regulation as summarized in Fig 2.
Mitochondria as an integrator of redox and O-GlcNAc signaling
It is well established that mitochondria play a central role in integrating cellular energy metabolism, redox signaling and cell survival pathways; however, the role of O-GlcNAcylation in regulating these processes is poorly understood. The notion that mitochondrial proteins might be potential targets for O-GlcNAc modification was first raised by the identification of a specific mitochondrial isoform of OGT (mOGT), which is localized to the inner membrane of mitochondria and contains mitochondrial targeting sequence [72]. While initial reports suggested that mOGT had either limited catalytic activity or that substrates for OGT in the mitochondria were very limited [11, 72], more recently, a number of studies have suggested that O-GlcNAcylation of mitochondria proteins contributes to both to acute cardioprotection [33, 38] as well as mitochondrial dysfunction and increased programmed cell death [45, 110].
Some of the first evidence to suggest that O-GlcNAc had a direct effect on mitochondrial function was the demonstration that acute increases in O-GlcNAc levels in the heart or in isolated cardiomyocytes, attenuated mPTP opening, a critical step in the initiation of programmed cell death [33, 38, 39, 149]. For example, mitochondria isolated from hearts of mice treated with the O-GlcNAcase inhibitor, PUGNAc were resistant to Ca2+-induced mPTP formation as assessed by mitochondrial swelling assay. Furthermore, overexpression of OGT in neonatal cardiomyocytes also decreased Ca2+-induced mitochondrial swelling; whereas, OGT inhibition increased mitochondrial swelling [38, 39]. VDAC has been identified as a potential O-GlcNAc target and it has been hypothesized that O-GlcNAcylation of VDAC preserves mitochondrial integrity by interfering with mPTP formation [38]. In addition we have shown that increasing overall O-GlcNAc levels either by increasing O-GlcNAc synthesis with glucosamine, and increased OGT expression or decreasing O-GlcNAc degradation by inhibiting O-GlcNAcase all attenuated H2O2-induced loss of mitochondrial membrane potential and cyctochrome c release [33], which was associated with increased mitochondrial Bcl-2 levels. Since Bcl-2 inhibits the mPTP opening possibly by interaction with VDAC, one of the putative components of mPTP [150, 151]. However, given that VDAC is not required for mPTP opening and the continued uncertainty regarding the molecular composition of the mPTP [152], whether O-GlcNAcylation of VDAC directly contributes to the attenuation of mPTP opening, has yet to be verified.
Despite the apparent protective effects associated with increasing mitochondrial O-GlcNAc levels, it was initially reported that overexpression of mOGT was toxic to cells [72]. More recently, Shin et al. [110] developed an inducible expression system enabling selective expression of either mOGT or ncOGT isoforms in mammalian cells. They reported that increasing mOGT levels induced apoptosis in both a human embryonic kidney fibroblast cell lime (EcR-293) and insulinoma derived INS-1 cell lines. The extent to which this would be applicable to the heart or cardiomyocytes is not known; however, given the high energetic demand of the heart and the importance of tight control of oxidative metabolism, it is likely that dysregulation of mitochondrial O-GlcNAcylation would also be detrimental to cardiomyocytes. Evidence in support of this was provided by Hu et al. [45], who reported that hyperglycemia induced mitochondrial dysfunction in cardiomyocyte was mediated via O-GlcNAcylation of mitochondrial proteins. Importantly they identified several mitochondrial proteins as targets for O-GlcNAc modification that are members of respiratory complexes, such as NDUFA9 of complex I, and the mitochondrial DNA-encoded, subunit I of Complex IV (COX I). They also found that hyperglycemia induced increases in mitochondrial O-GlcNAc levels resulted in impaired activity of Complex I, III and IV and that this could be reversed by increasing expression of O-GlcNAcase.
The study by Hu et al. [45] was the first to show that in cardiac mitochondria, proteins in the respiratory complexes are modified by O-GlcNAc and that this may contribute to impaired function induced by hyperglycemia. However, a number of key questions remain, including the regulation of mitochondrial O-GlcNAc synthesis and the mechanism by which removal of O-GlcNAc from mitochondrial proteins is catalyzed. Earlier reports speculated that the very low levels of mitochondrial O-GlcNAcylation could be due to limited substrate availability, i.e., UDP-GlcNAc [72]. The fact that even under basal conditions there was evidence of mitochondrial GlcNAcylation suggests that is not the case in the heart; however, this leaves open the question whether UDP-GlcNAc is actively transported into mitochondria, as it is in the ER and Golgi [153, 154] and the extent to which availability of UDP-GlcNAc is rate limiting for mitochondrial O-GlcNAc synthesis? Perhaps even more important for our understanding of O-GlcNAc cycling in the mitochondria is the mechanism by which O-GlcNAc is removed from mitochondrial proteins. Hu et al. [45] reported low levels of O-GlcNAcase activity in mitochondria isolated from mouse hearts and showed that increasing cellular levels of O-GlcNAcase attenuated the hyperglycemia induced increase in mitochondrial O-GlcNAc levels. However, as far as we are aware, no mitochondrial protein has been shown to have the hexosaminidase activity required to catalyze the removal of O-GlcNAc from proteins; in other words to date only one half of the O-GlcNAc cycle in the mitochondria, namely mOGT has been identified.
While is well established that hyperglycemia leads to increased O-GlcNAc levels in multiple cells and organs including the intact heart and cardiomyocytes, it is important to note that unlike glucosamine which is primarily metabolized via the HBP, increasing glucose levels has multiple effects, including increased oxidative stress. Indeed it has been reported that hyperglycemia leads to increase generation of mitochondrial superoxide and it is this increase in reactive oxygen species (ROS), which leads to activation of the HBP and increased O-GlcNAc synthesis [48, 49]. It has also been proposed that mitochondrial superoxide inhibits GAPDH, which further contributes to the increased flux of glucose through the HBP, by attenuated glycolysis [48, 49]. However, since relative little is known regarding the regulation of GFAT, OGT, and O-GlcNAcase, we cannot rule out the possibility that ROS could directly modulate their activities. Thus, hyperglycemia has the potential to increase O-GlcNAc levels both by directly increasing glucose flux through the HBP as well as by ROS mediated increase in pathways leading to O-GlcNAc synthesis.
While there are clearly many gaps in our knowledge regarding the regulation of mitochondrial O-GlcNAcylation it is increasingly evident that mitochondrial proteins are targets for O-GlcNAc modification. Our current understanding of effects of altered O-GlcNAc levels on mitochondria function is summarized in Fig 3. There is no doubt that in response to an acute stress, including oxidative stress there is an increase in cellular O-GlcNAc levels, and pharmacological approaches to augment this increase either by activating HBP flux or inhibiting O-GlcNAcase activity, increases tolerance of mitochondria to oxidative stress and thereby improves cell survival. In cardiomyocytes this increased tolerance to oxidative stress as discussed above is associated with increased O-GlcNAc levels on specific mitochondrial proteins, such as VDAC. In the case of a chronic stress such as that seen with hyperglycemia, there can be both a direct increase in O-GlcNAc synthesis due to increase glucose metabolism via the HBP as well as activation of the HBP mediated by increased mitochondrial ROS. Under sustained conditions, this has the potential to establish a feed forward loop where impaired mitochondrial function leads to greater ROS production and this could further augment the increase in O-GlcNAcylation, contributing to further mitochondrial dysfunction and ultimately cell death. Hu et al. [45] demonstrated that in cardiomyocytes there is a clear association between hyperglycemia, increased O-GlcNAcylation of key respiratory chain proteins and impaired mitochondrial function.
Figure 3. The intersection between O-GlcNAcylation, ROS and mitochondrial function.
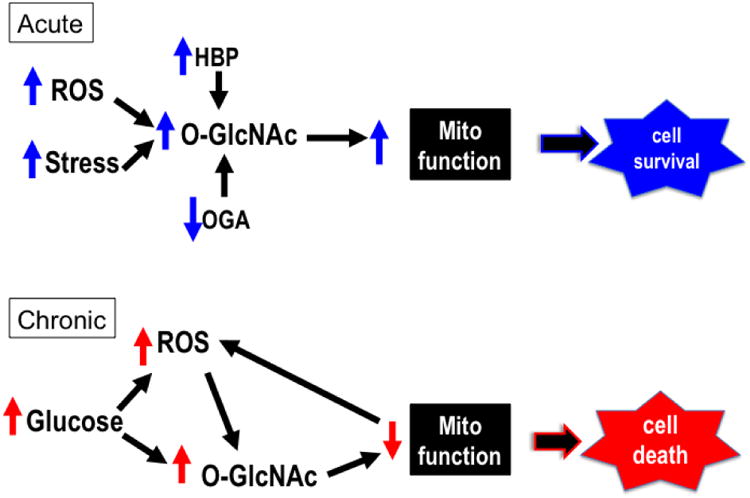
In response to an acute stress, including that induced by ROS, there is a rapid increase in cellular and potentially mitochondrial O-GlcNAcylation as a result of either an increased flux through the hexosamine biosynthesis pathway (HBP) and/or decreased O-GlcNAcase activity (OGA). This acute increase in O-GlcNAc levels has been shown to improve tolerance of mitochondria to oxidative stress and levels and attenuate loss of mitochondrial membrane potential leading to increased cell survival. Strategies designed to acutely augment this response have been shown to improve cell survival; conversely decreased O-GlcNAc levels lead to decreased cell survival. Chronic increases in cellular O-GlcNAc levels are typically associated with metabolic disease such as diabetes and the resulting hyperglycemia. Sustained increases in glucose levels can increase O-GlcNAc synthesis by directly increasing flux through the HBP as well as indirectly, as a result of hyperglycemia induced ROS production, which has also been shown to stimulate O-GlcNAc synthesis. Hyperglycemia is also known to lead to impaired mitochondrial function in part due to increased O-GlcNAcylation of mitochondrial proteins, which could in turn further increase ROS production and thereby in a feed forward manner continue to increase O-GlcNAc levels with even greater decline in mitochondria function. This O-GlcNAc mediated impairment of mitochondrial function, could then increase the vulnerability to additional stress thus leading to increased cell death. Indeed, targeted overexpression of mitochondrial OGT has been shown to lead to increased apoptosis.
The above discussion has focused on direct O-GlcNAc modification of mitochondrial proteins; however, it is should be recognized that changes in O-GlcNAc turnover may have indirect affects on mitochondrial function via O-GlcNAcylation of proteins that could influence mitochondrial function, but are not themselves mitochondrial proteins. One potentially intriguing example is GSK-3β, where increased O-GlcNAcylation attenuates its activity [76]. Furthermore, the cytoprotection associated with stress-induced increase in O-GlcNAc was reported to be due to increased heat shock protein expression as a consequence of O-GlcNAc-mediated inhibition of GSK-3β [30]. This is may be particularly relevant in the context of ischemic cardioprotection where GSK-3ß is a major convergence point for multiple cardioprotection strategies as well as a key effector for activation downstream targets [155-157], including attenuation of the mitochondrial permeability transition pore (mPTP).
O-GlcNAc and Redox Cell Signaling
In addition to being increased in response to various stress stimuli the generation of reactive oxygen species (ROS) is an inevitable byproduct of normal mitochondrial metabolism. Rather than just leading to non-specific modifications of lipids and proteins, it is widely recognized that ROS and reactive nitrogen species (RNS) play an integral role in regulating redox cell signaling pathways [158, 159]. An emerging concept in redox biology is the concept of “redox tone” [158, 159], where cell signaling, metabolism, and cell survival outcomes are linked to the antioxidant and thiol status of cells. Interestingly, several links between O-GlcNAc protein modification and oxidative stress suggest that O-GlcNAc signaling may represent an important mechanism that integrates both metabolic and redox signaling and thereby modulate redox tone.
One example of the intersection between redox signaling and O-GlcNAc is nitric oxide synthase (NOS), which is subject to both phosphorylation and O-GlcNAcylation and is responsible for the generation of nitric oxide (NO), one of the most widely recognized reactive species involved in redox signaling. Endothelial NOS (eNOS) is activated by Akt-mediated phosphorylation of Ser1177, which increases its activity; however this same site it also a target for O-GlcNAc modification, leading to lower activity and decreased NO production [49]. The interaction between O-GlcNAc and redox signaling can also occur at the transcriptional level; for example the transcription factor FoxO1, which is activated by O-GlcNAcylation [160] also regulates the transcription of oxidative stress responsive enzymes, such as catalase and MnSOD. Taken together these observations highlight the potential role of O-GlcNAc turnover integrating both acute and transcriptional responses to oxidative stress thereby playing a key role in regulating redox signaling.
Conclusions
Our understanding of the potential importance of protein O-GlcNAcylation in mediating the function and stress response of the heart and vascular system has only emerged over the past 5-10 years. This is highlighted by the fact that a PubMed search combining heart/cardiac/vascular with O-GlcNAc yields a total of only 65 papers, of which 51 or 78% have been published in the last 5 years. Studies to date have demonstrated that consistent with other tissues and organs changes in overall levels of O-GlcNAcylation occur rapidly in response to various stimuli emphasizing the dynamic nature of O-GlcNAc synthesis and removal. In agreement with much of the earlier literature on O-GlcNAcylation in other biological systems, increased O-GlcNAc levels have been linked to the adverse effects of metabolic disease, especially diabetes, on both cardiomyocyte and vascular function. There is also emerging evidence to suggest that dysregulation in O-GlcNAc cycling in vascular smooth muscle may be associated with hypertension; however, further work is needed to establish a true causal relationship. There is also substantial evidence demonstrating that acute augmentation of cardiac O-GlcNAc levels either by increasing synthesis or inhibiting degradation affords significant ischemic cardioprotection and this has been demonstrated at cellular level, the perfused heart and in vivo. While much of the emphasis on studies of O-GlcNAcylation in the heart have been focused on its role in mediating the response to various pathophysiological stresses, recent data has emerged demonstrating that acute and relatively subtle changes in O-GlcNAcylation can directly modulate cardiac metabolism, illustrating that it also contribute to the regulation of normal physiological processes.
Parallels are frequently drawn between phosphorylation and O-GlcNAcylation, and while this is not surprising given that both respond rapidly to wide range of stimuli and modify similar protein residues via an O-linkage, there are however some notable differences. The most obvious difference is that in contrast to the hundreds of kinases and phosphatases involved in regulating phosphorylation, there is a single OGT responsible for adding O-GlcNAc to proteins and single OGA to remove O-GlcNAc. This raises a key question as to how the kind of specificity associated with phosphorylation can be achieved with O-GlcNAcylation? One putative mechanism is the multiple TPRs in the N-terminal domain of OGT, which play a key role in recognition and activation of specific protein targets [59, 76]. In support of this there are clear examples of OGT forming transient complexes with key protein targets in response to specific stimuli [74, 87]; however considerable work remains, to better understand the activation and regulation of the formation of these protein complexes/
Given that O-GlcNAcylation appears to be as abundant and phosphorylation, it is perhaps surprising that its not as widely studied. It is worth remembering, however, that the recognition of phosphorylation as an important mechanism for regulating protein function took many decades to be fully appreciated. As discussed by Krebs in his 1992 Novel lecture, whilethe discovery of serine/threonine phosphorylation occurred as early as 1933; it was only by1968 that it was recognized that phosphorylation could be regulated by extracellular stimuli [161] and by 1976, 43 years after it was first described, the number of enzymes known toundergo phosphorylation/dephosphorylation was over 20 [161]. It is now a little over 25 yearssince protein O-GlcNAcylation was first described [2] and currently more than 1000 proteinshave been identified as being targets for this modification(http://cbsb.lombardi.georgetown.edu/statistic.php). One reason why studies of O-GlcNAcylation have not emerged more rapidly is due, at least in part, because that it is a low molecular weight modification and unlike phosphorylation is uncharged, therefore does not lead to gel shifts. In addition it is very labile not only in traditional MS analyses, but also if tissue samples are processed without O-GlcNAcase inhibitors, it is readily lost from proteins, as would occur with phosphorylation in the absence of phosphatase inhibitors. Finally, the lack of available reagents has also been a hindrance; until very recently, there were only 2 commercially available pan O-GlcNAc antibodies (CTD110.6 and RL2) and antibodies to OGT and OGA have only become widely available in the past 3-5 years. In addition a critical limitation in trying to elucidate O-GlcNAc dependent signaling networks is the lack of site specific O-GlcNAc antibodies. Antibodies generated against synthetic O-GlcNAcylated peptides have provided site-specific (S1011-O-GlcNAc IRS-1 [108]) and pan-specific (CTD110.6) antibodies; however, the synthesis and deprotection of O-GlcNAc peptides is significantly more challenging than that of phosphopeptides.
It is clear that O-GlcNAcylation is an integral component of the complex signaling network involved in regulating cellular responses to physiological and pathophysiological stimuli; however, it is also equally clear that our understanding of the fundamental mechanisms involved in regulating O-GlcNAc turnover is surprisingly limited. A major challenge has been the lack of reliable tools, including antibodies, which are taken for granted in the investigation of many PTMs; however, as the methods for identifying and characterizing O-GlcNAcylated proteins are continuing to improve and become more widely available, it is anticipated that there will be an increasing number of investigators driven to elucidate more fully the role of O-GlcNAc signaling in the cardiovascular system.
Table 1.
Methods Utilized for the Characterization of O-GlcNAc Modified Proteins.
| Methodology for the detection of O-GlcNAc modified proteins | O-GlcNAcylated proteins identified (No.) | Identification of O-GlcNAc modification site (No.) | Compatible with quantitative methods | References | Tissue or cell type |
|---|---|---|---|---|---|
| Anti-O-GlcNAc Immunoprecipitation and detection by LC-MS/MS with CID or ETD. | Yes (215) | No | Yes | [111] | HEK293 cells |
| Yes (51) | No | Yes (SILAC) | [164] | Cos-7 cells | |
| Lectin Weak Affinity Chromatography (LWAC) and detection by LC MS/MS with ETD | Yes | Yes (145) | [126] | Brain Cortex | |
| Yes | Yes (58) | [127]* | Brain Cortex | ||
| Yes | Yes | Yes (iTRAQ) | [129] | Brain | |
| Yes (62) | Yes (142) | Yes (SILAC) | [131] | Embryonic stem cells | |
| Chemoenzymatic labeling: Enzymatic incorporation of a reactive sugar analog followed by click chemistry. Detection by LC-MSMS with CID or ETD. | Yes (25) | No | [165] | Brain | |
| Yes (20) | No | [166] | Xenopus oocytes | ||
| Yes (pilot study) | Yes (ETD) | [167] | Brain | ||
| Yes (32) | No | [115] | MCF-7 cells | ||
| Yes (25) | Yes (BEMAD) | Yes (iTRAQ) | [130] | Erthyrocytes | |
| Chemoenzymatic labeling: Enzymatic incorporation of a reactive sugar analog followed by click chemistry with a photocleavable biotin linker. Detection by LC MS/MS with ETD. | Yes (64) | Yes (141) | Yes (SILAC) | [132]* | Hela cells |
| Metabolic labeling in intact cells followed by gel-based separation and LC-MS/MS | Yes (199) | No | Yes | [116] | Hela cells |
| Yes (pilot study) | No | No | [119] | Jurkat cells | |
| Yes (374) | No | No | [120] | NIH-3T3 cells |
Highlights.
- Proteins O-GlcNAcylation regulates of cardiomyocyte stress response
- Increased O-GlcNAc levels linked to both cardioprotection and diabetic complications
- O-GlcNAcylation is a novel mechanism for regulation of cardiac metabolism
- Mitochondrial proteins are targets for O-GlcNAcylation
- New technologies will facilitate characterization of O-GlcNAcylated proteins
Acknowledgments
This work was supported by NIH R01 Grants ES10167, AA13395, DK075867 to VDU; DE020925 to LEB; HL101192 and HL079364 to JCC.
Footnotes
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Spiro RG. Protein glycosylation: nature, distribution, enzymatic formation, and disease implications of glycopeptide bonds. Glycobiology. 2002;12:43R–56R. doi: 10.1093/glycob/12.4.43r. [DOI] [PubMed] [Google Scholar]
- 2.Torres CR, Hart GW. Topography and polypeptide distribution of terminal N-acetylglucosamine residues on the surfaces of intact lymphocytes. Evidence for O-linked GlcNAc. J Biol Chem. 1984;259:3308–17. [PubMed] [Google Scholar]
- 3.Hu P, Shimoji S, Hart GW. Site-specific interplay between O-GlcNAcylation and phosphorylation in cellular regulation. FEBS letters. 2010;584:2526–38. doi: 10.1016/j.febslet.2010.04.044. [DOI] [PubMed] [Google Scholar]
- 4.Zeidan Q, Hart GW. The intersections between O-GlcNAcylation and phosphorylation: implications for multiple signaling pathways. J Cell Sci. 2010;123:13–22. doi: 10.1242/jcs.053678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butkinaree C, Park K, Hart GW. O-linked beta-N-acetylglucosamine (O-GlcNAc): Extensive crosstalk with phosphorylation to regulate signaling and transcription in response to nutrients and stress. Biochim Biophys Acta. 2010;1800:96–106. doi: 10.1016/j.bbagen.2009.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanover JA, Krause MW, Love DC. The hexosamine signaling pathway: O-GlcNAc cycling in feast or famine. Biochim Biophys Acta. 2010;1800:80–95. doi: 10.1016/j.bbagen.2009.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hart GW, Slawson C, Ramirez-Correa G, Lagerlof O. Cross Talk Between O-GlcNAcylation and Phosphorylation: Roles in Signaling, Transcription, and Chronic Disease. Annu Rev Biochem. 2010 doi: 10.1146/annurev-biochem-060608-102511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slawson C, Housley MP, Hart GW. O-GlcNAc cycling: How a single sugar post-translational modification is changing the Way We think about signaling networks. J Cell Biochem. 2006;97:71–83. doi: 10.1002/jcb.20676. [DOI] [PubMed] [Google Scholar]
- 9.Zachara NE, Hart GW. O-GlcNAc a sensor of cellular state: the role of nucleocytoplasmic glycosylation in modulating cellular function in response to nutrition and stress. Biochim Biophys Acta. 2004;1673:13–28. doi: 10.1016/j.bbagen.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 10.Zachara NE, Hart GW. Cell signaling, the essential role of O-GlcNAc! Biochim Biophys Acta. 2006;1761:599–617. doi: 10.1016/j.bbalip.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Love DC, Hanover JA. The hexosamine signaling pathway: deciphering the “O-GlcNAc code”. Sci STKE. 2005;2005:re13. doi: 10.1126/stke.3122005re13. [DOI] [PubMed] [Google Scholar]
- 12.Zachara NE, Hart GW. O-GlcNAc modification: a nutritional sensor that modulates proteasome function. Trends Cell Biol. 2004;14:218–21. doi: 10.1016/j.tcb.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Han I, Kudlow JE. Reduced O glycosylation of Sp1 is associated with increased proteasome susceptibility. Mol Cell Biol. 1997;17:2550–8. doi: 10.1128/mcb.17.5.2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells L, Whalen SA, Hart GW. O-GlcNAc: a regulatory post-translational modification. Biochem Biophys Res Commun. 2003;302:435–41. doi: 10.1016/s0006-291x(03)00175-x. [DOI] [PubMed] [Google Scholar]
- 15.Liu K, Paterson AJ, Zhang F, McAndrew J, Fukuchi K, Wyss JM, et al. Accumulation of protein O-GlcNAc modification inhibits proteasomes in the brain and coincides with neuronal apoptosis in brain areas with high O-GlcNAc metabolism. J Neurochem. 2004;89:1044–55. doi: 10.1111/j.1471-4159.2004.02389.x. [DOI] [PubMed] [Google Scholar]
- 16.Guinez C, Morelle W, Michalski JC, Lefebvre T. O-GlcNAc glycosylation: a signal for the nuclear transport of cytosolic proteins? Int J Biochem Cell Biol. 2005;37:765–74. doi: 10.1016/j.biocel.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Comer FI, Hart GW. O-GlcNAc and the control of gene expression. Biochim Biophys Acta. 1999;1473:161–71. doi: 10.1016/s0304-4165(99)00176-2. [DOI] [PubMed] [Google Scholar]
- 18.Chou TY, Hart GW, Dang CV. c-Myc is glycosylated at threonine 58, a known phosphorylation site and a mutational hot spot in lymphomas. J Biol Chem. 1995;270:18961–5. doi: 10.1074/jbc.270.32.18961. [DOI] [PubMed] [Google Scholar]
- 19.Shaw P, Freeman J, Bovey R, Iggo R. Regulation of specific DNA binding by p53: evidence for a role for O-glycosylation and charged residues at the carboxy-terminus. Oncogene. 1996;12:921–30. [PubMed] [Google Scholar]
- 20.Donadio AC, Lobo C, Tosina M, de la Rosa V, Martin-Rufian M, Campos-Sandoval JA, et al. Antisense glutaminase inhibition modifies the O-GlcNAc pattern and flux through the hexosamine pathway in breast cancer cells. J Cell Biochem. 2008;103:800–11. doi: 10.1002/jcb.21449. [DOI] [PubMed] [Google Scholar]
- 21.Fulop N, Mason MM, Dutta K, Wang P, Davidoff AJ, Marchase RB, et al. The impact of Type-2 diabetes and aging on cardiomyocyte function and O-Linked N-acetylglucosamine levels in the heart. Am J Physiol Cell Physiol. 2007;292:C1370–8. doi: 10.1152/ajpcell.00422.2006. [DOI] [PubMed] [Google Scholar]
- 22.Rex-Mathes M, Werner S, Strutas D, Griffith LS, Viebahn C, Thelen K, et al. O-GlcNAc expression in developing and ageing mouse brain. Biochimie. 2001;83:583–90. doi: 10.1016/s0300-9084(01)01305-0. [DOI] [PubMed] [Google Scholar]
- 23.Fulop N, Feng W, Xing D, He K, Not LG, Brocks CA, et al. Aging leads to increased levels of protein O-linked N-acetylglucosamine in heart, aorta, brain and skeletal muscle in Brown-Norway rats. Biogerontology. 2008;9:139–51. doi: 10.1007/s10522-007-9123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hanover JA. Glycan-dependent signaling: O-linked N-acetylglucosamine. FASEB J. 2001;15:1865–76. doi: 10.1096/fj.01-0094rev. [DOI] [PubMed] [Google Scholar]
- 25.Dias WB, Hart GW. O-GlcNAc modification in diabetes and Alzheimer's disease. Mol Biosyst. 2007;3:766–72. doi: 10.1039/b704905f. [DOI] [PubMed] [Google Scholar]
- 26.Buse MG. Hexosamines, insulin resistance, and the complications of diabetes: current status. Am J Physiol Endocrinol Metab. 2006;290:E1–E8. doi: 10.1152/ajpendo.00329.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Copeland RJ, Bullen JW, Hart GW. Cross-talk between GlcNAcylation and phosphorylation: roles in insulin resistance and glucose toxicity. Am J Physiol Endocrinol Metab. 2008;295:E17–28. doi: 10.1152/ajpendo.90281.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Donnell N, Zachara NE, Hart GW, Marth JD. Ogt-dependent X-chromosome-linked protein glycosylation is a requisite modification in somatic cell function and embryo viability. Mol Cell Biol. 2004;24:1680–90. doi: 10.1128/MCB.24.4.1680-1690.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zachara NE, O'Donnell N, Cheung WD, Mercer JJ, Marth JD, Hart GW. Dynamic O-GlcNAc modification of nucleocytoplasmic proteins in response to stress. A survival response of mammalian cells. J Biol Chem. 2004;279:30133–42. doi: 10.1074/jbc.M403773200. [DOI] [PubMed] [Google Scholar]
- 30.Kazemi Z, Chang H, Haserodt S, McKen C, Zachara NE. O-linked beta-N-acetylglucosamine (O-GlcNAc) regulates stress-induced heat shock protein expression in a GSK-3beta-dependent manner. The Journal of biological chemistry. 2010;285:39096–107. doi: 10.1074/jbc.M110.131102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu J, Marchase RB, Chatham JC. Increased O-GlcNAc levels during reperfusion lead to improved functional recovery and reduced calpain proteolysis. Am J Physiol Heart Circ Physiol. 2007;293:H1391–9. doi: 10.1152/ajpheart.00285.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu J, Pang Y, Chang T, Bounelis P, Chatham JC, Marchase RB. Increased hexosamine biosynthesis and protein O-GlcNAc levels associated with myocardial protection against calcium paradox and ischemia. J Mol Cell Cardiol. 2006;40:303–12. doi: 10.1016/j.yjmcc.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 33.Champattanachai V, Marchase RB, Chatham JC. Glucosamine protects neonatal cardiomyocytes from ischemia-reperfusion injury via increased protein O-GlcNAc and increased mitochondrial Bcl-2. Am J Physiol Cell Physiol. 2008;294:C1509–20. doi: 10.1152/ajpcell.00456.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Champattanachai V, Marchase RB, Chatham JC. Glucosamine protects neonatal cardiomyocytes from ischemia-reperfusion injury via increased protein-associated O-GlcNAc. Am J Physiol Cell Physiol. 2007;292:C178–87. doi: 10.1152/ajpcell.00162.2006. [DOI] [PubMed] [Google Scholar]
- 35.Champattanachai V, Marchase RB, Chatham JC. Glucosamine protects neonatal cardiomyocytes from ischemia-reperfusion injury through translocation of Bcl2 family proteins. Faseb J. 2007;21:746–14. [Google Scholar]
- 36.Fulop N, Zhang Z, Marchase RB, Chatham JC. Glucosamine cardioprotection in perfused rat hearts associated with increased O-linked N-acetylglucosamine protein modification and altered p38 activation. Am J Physiol Heart Circ Physiol. 2007;292:H2227–36. doi: 10.1152/ajpheart.01091.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laczy B, Marsh SA, Brocks CA, Wittmann I, Chatham JC. Inhibition of O-GlcNAcase in perfused rat hearts by NAG-thiazolines at the time of reperfusion is cardioprotective in an O-GlcNAc-dependent manner. Am J Physiol Heart Circ Physiol. 2010;299:H1715–27. doi: 10.1152/ajpheart.00337.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones SP, Zachara NE, Ngoh GA, Hill BG, Teshima Y, Bhatnagar A, et al. Cardioprotection by N-acetylglucosamine linkage to cellular proteins. Circulation. 2008;117:1172–82. doi: 10.1161/CIRCULATIONAHA.107.730515. [DOI] [PubMed] [Google Scholar]
- 39.Ngoh GA, Watson LJ, Facundo HT, Dillmann W, Jones SP. Non-canonical glycosyltransferase modulates post-hypoxic cardiac myocyte death and mitochondrial permeability transition. J Mol Cell Cardiol. 2008;45:313–25. doi: 10.1016/j.yjmcc.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ngoh GA, Facundo HT, Hamid T, Dillmann W, Zachara NE, Jones SP. Unique hexosaminidase reduces metabolic survival signal and sensitizes cardiac myocytes to hypoxia/reoxygenation injury. Circ Res. 2009;104:41–9. doi: 10.1161/CIRCRESAHA.108.189431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu T, Zhou H, Jin Z, Bi S, Yang X, Yi D, et al. Cardioprotection of salidroside from ischemia/reperfusion injury by increasing N-acetylglucosamine linkage to cellular proteins. Eur J Pharmacol. 2009;613:93–9. doi: 10.1016/j.ejphar.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 42.Xing D, Feng W, Not LG, Miller AP, Zhang Y, Chen YF, et al. Increased protein O-GlcNAc modification inhibits inflammatory and neointimal responses to acute endoluminal arterial injury. Am J Physiol Heart Circ Physiol. 2008;295:H335–42. doi: 10.1152/ajpheart.01259.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clark RJ, McDonough PM, Swanson E, Trost SU, Suzuki M, Fukuda M, et al. Diabetes and the accompanying hyperglycemia impairs cardiomyocyte cycling through increased nuclear O-GlcNAcylation. J Biol Chem. 2003;278:44230–7. doi: 10.1074/jbc.M303810200. [DOI] [PubMed] [Google Scholar]
- 44.Hu Y, Belke D, Suarez J, Swanson E, Clark R, Hoshijima M, et al. Adenovirus-mediated overexpression of O-GlcNAcase improves contractile function in the diabetic heart. Circ Res. 2005;96:1006–13. doi: 10.1161/01.RES.0000165478.06813.58. [DOI] [PubMed] [Google Scholar]
- 45.Hu Y, Suarez J, Fricovsky E, Wang H, Scott BT, Trauger SA, et al. Increased enzymatic O-GlcNAcylation of mitochondrial proteins impairs mitochondrial function in cardiac myocytes exposed to high glucose. J Biol Chem. 2009;284:547–55. doi: 10.1074/jbc.M808518200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marsh SA, Dell'Italia LJ, Chatham JC. Activation of the hexosamine biosynthesis pathway and protein O-GlcNAcylation modulate hypertrophic and cell signaling pathways in cardiomyocytes from diabetic mice. Amino Acids. 2011;40:819–28. doi: 10.1007/s00726-010-0699-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pang Y, Bounelis P, Chatham JC, Marchase RB. Hexosamine pathway is responsible for inhibition by diabetes of phenylephrine-induced inotropy. Diabetes. 2004;53:1074–81. doi: 10.2337/diabetes.53.4.1074. [DOI] [PubMed] [Google Scholar]
- 48.Du XL, Edelstein D, Rossetti L, Fantus IG, Goldberg H, Ziyadeh F, et al. Hyperglycemia-induced mitochondrial superoxide overproduction activates the hexosamine pathway and induces plasminogen activator inhibitor-1 expression by increasing Sp1 glycosylation. Proc Natl Acad Sci U S A. 2000;97:12222–6. doi: 10.1073/pnas.97.22.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Du XL, Edelstein D, Dimmeler S, Ju Q, Sui C, Brownlee M. Hyperglycemia inhibits endothelial nitric oxide synthase activity by posttranslational modification at the Akt site. J Clin Invest. 2001;108:1341–8. doi: 10.1172/JCI11235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lima VV, Giachini FR, Carneiro FS, Carneiro ZN, Saleh MA, Pollock DM, et al. O-GlcNAcylation contributes to augmented vascular reactivity induced by endothelin 1. Hypertension. 2010;55:180–8. doi: 10.1161/HYPERTENSIONAHA.109.143818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lima VV, Giachini FR, Carneiro FS, Carvalho MH, Fortes ZB, Webb RC, et al. O-GlcNAcylation contributes to the vascular effects of ET-1 via activation of the RhoA/Rho-kinase pathway. Cardiovasc Res. 2011;89:614–22. doi: 10.1093/cvr/cvq338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lima VV, Giachini FR, Hardy DM, Webb RC, Tostes RC. O-GlcNAcylation: a novel pathway contributing to the effects of endothelin in the vasculature. Am J Physiol Regul Integr Comp Physiol. 2011;300:R236–50. doi: 10.1152/ajpregu.00230.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lima VV, Rigsby CS, Hardy DM, Webb RC, Tostes RC. O-GlcNAcylation: a novel post-translational mechanism to alter vascular cellular signaling in health and disease: focus on hypertension. J Am Soc Hypertens. 2009;3:374–87. doi: 10.1016/j.jash.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chatham JC, Marchase RB. The role of protein O-linked beta-N-acetylglucosamine in mediating cardiac stress responses. Biochim Biophys Acta. 2010;1800:57–66. doi: 10.1016/j.bbagen.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fulop N, Marchase RB, Chatham JC. Role of protein O-linked N-acetyl-glucosamine in mediating cell function and survival in the cardiovascular system. Cardiovasc Res. 2007;73:288–97. doi: 10.1016/j.cardiores.2006.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ngoh GA, Facundo HT, Zafir A, Jones SP. O-GlcNAc signaling in the cardiovascular system. Circ Res. 2010;107:171–85. doi: 10.1161/CIRCRESAHA.110.224675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Whelan SA, Hart GW. Proteomic approaches to analyze the dynamic relationships between nucleocytoplasmic protein glycosylation and phosphorylation. Circ Res. 2003;93:1047–58. doi: 10.1161/01.RES.0000103190.20260.37. [DOI] [PubMed] [Google Scholar]
- 58.Ngoh GA, Jones SP. New insights into metabolic signaling and cell survival: the role of beta-O-linkage of N-acetylglucosamine. J Pharmacol Exp Ther. 2008;327:602–9. doi: 10.1124/jpet.108.143263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kreppel LK, Hart GW. Regulation of a cytosolic and nuclear O-GlcNAc transferase. Role of the tetratricopeptide repeats. J Biol Chem. 1999;274:32015–22. doi: 10.1074/jbc.274.45.32015. [DOI] [PubMed] [Google Scholar]
- 60.Kornfeld R. Studies on L-glutamine D-fructose 6-phosphate amidotransferase. I. Feedback inhibition by uridine diphosphate-N-acetylglucosamine. J Biol Chem. 1967;242:3135–41. [PubMed] [Google Scholar]
- 61.Marshall S, Bacote V, Traxinger RR. Complete inhibition of glucose-induced desensitization of the glucose transport system by inhibitors of mRNA synthesis. Evidence for rapid turnover of glutamine:fructose-6-phosphate amidotransferase. J Biol Chem. 1991;266:10155–61. [PubMed] [Google Scholar]
- 62.Oki T, Yamazaki K, Kuromitsu J, Okada M, Tanaka I. cDNA cloning and mapping of a novel subtype of glutamine:fructose-6-phosphate amidotransferase (GFAT2) in human and mouse. Genomics. 1999;57:227–34. doi: 10.1006/geno.1999.5785. [DOI] [PubMed] [Google Scholar]
- 63.Young ME, Yan J, Razeghi P, Cooksey RC, Guthrie PH, Stepkowski SM, et al. Proposed regulation of gene expression by glucose in rodent heart. Gene Reg Systems Biol. 2007;1:251–62. doi: 10.4137/grsb.s222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chang Q, Su K, Baker JR, Yang X, Paterson AJ, Kudlow JE. Phosphorylation of human glutamine:fructose-6-phosphate amidotransferase by cAMP-dependent protein kinase at serine 205 blocks the enzyme activity. J Biol Chem. 2000;275:21981–7. doi: 10.1074/jbc.M001049200. [DOI] [PubMed] [Google Scholar]
- 65.Hu Y, Riesland L, Paterson AJ, Kudlow JE. Phosphorylation of mouse glutamine-fructose-6-phosphate amidotransferase 2 (GFAT2) by cAMP-dependent protein kinase increases the enzyme activity. J Biol Chem. 2004;279:29988–93. doi: 10.1074/jbc.M401547200. [DOI] [PubMed] [Google Scholar]
- 66.Li Y, Roux C, Lazereg S, LeCaer JP, Laprevote O, Badet B, et al. Identification of a novel serine phosphorylation site in human glutamine:fructose-6-phosphate amidotransferase isoform 1. Biochemistry. 2007;46:13163–9. doi: 10.1021/bi700694c. [DOI] [PubMed] [Google Scholar]
- 67.Boehmelt G, Wakeham A, Elia A, Sasaki T, Plyte S, Potter J, et al. Decreased UDP-GlcNAc levels abrogate proliferation control in EMeg32-deficient cells. Embo J. 2000;19:5092–104. doi: 10.1093/emboj/19.19.5092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Greig KT, Antonchuk J, Metcalf D, Morgan PO, Krebs DL, Zhang JG, et al. Agm1/Pgm3-mediated sugar nucleotide synthesis is essential for hematopoiesis and development. Mol Cell Biol. 2007;27:5849–59. doi: 10.1128/MCB.00802-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nolte D, Muller U. Human O-GlcNAc transferase (OGT): genomic structure, analysis of splice variants, fine mapping in Xq13.1. Mamm Genome. 2002;13:62–4. doi: 10.1007/s00335-001-2108-9. [DOI] [PubMed] [Google Scholar]
- 70.Hanover JA, Yu S, Lubas WB, Shin SH, Ragano-Caracciola M, Kochran J, et al. Mitochondrial and nucleocytoplasmic isoforms of O-linked GlcNAc transferase encoded by a single mammalian gene. Arch Biochem Biophys. 2003;409:287–97. doi: 10.1016/s0003-9861(02)00578-7. [DOI] [PubMed] [Google Scholar]
- 71.Kreppel LK, Blomberg MA, Hart GW. Dynamic glycosylation of nuclear and cytosolic proteins. Cloning and characterization of a unique O-GlcNAc transferase with multiple tetratricopeptide repeats. J Biol Chem. 1997;272:9308–15. doi: 10.1074/jbc.272.14.9308. [DOI] [PubMed] [Google Scholar]
- 72.Love DC, Kochan J, Cathey RL, Shin SH, Hanover JA, Kochran J. Mitochondrial and nucleocytoplasmic targeting of O-linked GlcNAc transferase. J Cell Sci. 2003;116:647–54. doi: 10.1242/jcs.00246. [DOI] [PubMed] [Google Scholar]
- 73.Haltiwanger RS, Blomberg MA, Hart GW. Glycosylation of nuclear and cytoplasmic proteins. Purification and characterization of a uridine diphospho-N- acetylglucosamine:polypeptide beta-N-acetylglucosaminyltransferase. J Biol Chem. 1992;267:9005–13. [PubMed] [Google Scholar]
- 74.Yang X, Ongusaha PP, Miles PD, Havstad JC, Zhang F, So WV, et al. Phosphoinositide signalling links O-GlcNAc transferase to insulin resistance. Nature. 2008;451:964–9. doi: 10.1038/nature06668. [DOI] [PubMed] [Google Scholar]
- 75.Whelan SA, Lane MD, Hart GW. Regulation of the O-linked beta-N-acetylglucosamine transferase by insulin signaling. J Biol Chem. 2008;283:21411–7. doi: 10.1074/jbc.M800677200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lubas WA, Hanover JA. Functional expression of O-linked GlcNAc transferase. Domain structure and substrate specificity. J Biol Chem. 2000;275:10983–8. doi: 10.1074/jbc.275.15.10983. [DOI] [PubMed] [Google Scholar]
- 77.Dong DL, Hart GW. Purification and characterization of an O-GlcNAc selective N-acetyl-beta-D-glucosaminidase from rat spleen cytosol. J Biol Chem. 1994;269:19321–30. [PubMed] [Google Scholar]
- 78.Gao Y, Wells L, Comer FI, Parker GJ, Hart GW. Dynamic O-glycosylation of nuclear and cytosolic proteins: cloning and characterization of a neutral, cytosolic beta-N-acetylglucosaminidase from human brain. J Biol Chem. 2001;276:9838–45. doi: 10.1074/jbc.M010420200. [DOI] [PubMed] [Google Scholar]
- 79.Kim EJ, Kang DO, Love DC, Hanover JA. Enzymatic characterization of O-GlcNAcase isoforms using a fluorogenic GlcNAc substrate. Carbohydr Res. 2006;341:971–82. doi: 10.1016/j.carres.2006.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wells L, Gao Y, Mahoney JA, Vosseller K, Chen C, Rosen A, et al. Dynamic O-glycosylation of nuclear and cytosolic proteins: further characterization of the nucleocytoplasmic beta-N-acetylglucosaminidase, O-GlcNAcase. J Biol Chem. 2002;277:1755–61. doi: 10.1074/jbc.m109656200. [DOI] [PubMed] [Google Scholar]
- 81.Toleman C, Paterson AJ, Whisenhunt TR, Kudlow JE. Characterization of the histone acetyltransferase (HAT) domain of a bifunctional protein with activable O-GlcNAcase and HAT activities. J Biol Chem. 2004;279:53665–73. doi: 10.1074/jbc.M410406200. [DOI] [PubMed] [Google Scholar]
- 82.Butkinaree C, Cheung WD, Park S, Park K, Barber M, Hart GW. Characterization of beta-N-acetylglucosaminidase cleavage by caspase-3 during apoptosis. J Biol Chem. 2008;283:23557–66. doi: 10.1074/jbc.M804116200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kneass ZT, Marchase RB. Neutrophils exhibit rapid agonist-induced increases in protein-associated O-GlcNAc. J Biol Chem. 2004;279:45759–65. doi: 10.1074/jbc.M407911200. [DOI] [PubMed] [Google Scholar]
- 84.Song M, Kim HS, Park JM, Kim SH, Kim IH, Ryu SH, et al. o-GlcNAc transferase is activated by CaMKIV-dependent phosphorylation under potassium chloride-induced depolarization in NG-108-15 cells. Cell Signal. 2008;20:94–104. doi: 10.1016/j.cellsig.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 85.Wang Z, Gucek M, Hart GW. Cross-talk between GlcNAcylation and phosphorylation: site-specific phosphorylation dynamics in response to globally elevated O-GlcNAc. Proc Natl Acad Sci U S A. 2008;105:13793–8. doi: 10.1073/pnas.0806216105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wells L, Kreppel LK, Comer FI, Wadzinski BE, Hart GW. O-GlcNAc transferase is in a functional complex with protein phosphatase 1 catalytic subunits. J Biol Chem. 2004;279:38466–70. doi: 10.1074/jbc.M406481200. [DOI] [PubMed] [Google Scholar]
- 87.Slawson C, Lakshmanan T, Knapp S, Hart GW. A mitotic GlcNAcylation/phosphorylation signaling complex alters the posttranslational state of the cytoskeletal protein vimentin. Mol Biol Cell. 2008;19:4130–40. doi: 10.1091/mbc.E07-11-1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Milewski S. Glucosamine-6-phosphate synthase - the multi-facets enzyme. Biochim Biophys Acta. 2002;1597:173–92. doi: 10.1016/s0167-4838(02)00318-7. [DOI] [PubMed] [Google Scholar]
- 89.Uldry M, Ibberson M, Hosokawa M, Thorens B. GLUT2 is a high affinity glucosamine transporter. FEBS Lett. 2002;524:199–203. doi: 10.1016/s0014-5793(02)03058-2. [DOI] [PubMed] [Google Scholar]
- 90.Laczy B, Fulop N, Onay-Besikci A, Des Rosiers C, Chatham JC. Acute regulation of cardiac metabolism by the hexosamine biosynthesis pathway and protein O-GlcNAcylation. PLoS One. 2011;6:e18417. doi: 10.1371/journal.pone.0018417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Masson E, Wiernsperger N, Lagarde M, El Bawab S. Glucosamine induces cell-cycle arrest and hypertrophy of mesangial cells: implication of gangliosides. Biochem J. 2005;388:537–44. doi: 10.1042/BJ20041506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Stanley P. A method to the madness of N-glycan complexity? Cell. 2007;129:27–9. doi: 10.1016/j.cell.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 93.Virkamaki A, Yki-Jarvinen H. Allosteric regulation of glycogen synthase and hexokinase by glucosamine-6-phosphate during glucosamine-induced insulin resistance in skeletal muscle and heart. Diabetes. 1999;48:1101–7. doi: 10.2337/diabetes.48.5.1101. [DOI] [PubMed] [Google Scholar]
- 94.Zou L, Yang S, Champattanachai V, Hu S, Chaudry IH, Marchase RB, et al. Glucosamine improves cardiac function following trauma-hemorrhage by increased protein O-GlcNAcylation and attenuation of NF-{kappa}B signaling. Am J Physiol Heart Circ Physiol. 2009;296:H515–23. doi: 10.1152/ajpheart.01025.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Marshall S, Nadeau O, Yamasaki K. Dynamic actions of glucose and glucosamine on hexosamine biosynthesis in isolated adipocytes: differential effects on glucosamine 6-phosphate, UDP-N-acetylglucosamine, and ATP levels. J Biol Chem. 2004;279:35313–9. doi: 10.1074/jbc.M404133200. [DOI] [PubMed] [Google Scholar]
- 96.Haltiwanger RS, Grove K, Philipsberg GA. Modulation of O-linked N-acetylglucosamine levels on nuclear and cytoplasmic proteins in vivo using the peptide O-GlcNAc-beta-N-acetylglucosaminidase inhibitor O-(2-acetamido-2-deoxy-D-glucopyranosylidene)amino-N-phenylcarbamate. J Biol Chem. 1998;273:3611–7. doi: 10.1074/jbc.273.6.3611. [DOI] [PubMed] [Google Scholar]
- 97.Shanmugasundaram B, Debowski AW, Dennis RJ, Davies GJ, Vocadlo DJ, Vasella A. Inhibition of O-GlcNAcase by a gluco-configured nagstatin and a PUGNAc-imidazole hybrid inhibitor. Chem Commun (Camb) 2006:4372–4. doi: 10.1039/b612154c. [DOI] [PubMed] [Google Scholar]
- 98.Zou LY, Yang S, Chaudry IH, Marchase RB, Chatham JC. PUGNAc administration during resuscitation improves organ function following trauma-hemorrhage. Shock. 2007;27:402–8. doi: 10.1097/01.shk.0000209563.07693.db. [DOI] [PubMed] [Google Scholar]
- 99.Macauley MS, Whitworth GE, Debowski AW, Chin D, Vocadlo DJ. O-GlcNAcase uses substrate-assisted catalysis: kinetic analysis and development of highly selective mechanism-inspired inhibitors. J Biol Chem. 2005;280:25313–22. doi: 10.1074/jbc.M413819200. [DOI] [PubMed] [Google Scholar]
- 100.Dorfmueller HC, Borodkin VS, Schimpl M, Shepherd SM, Shpiro NA, van Aalten DM. GlcNAcstatin: a picomolar, selective O-GlcNAcase inhibitor that modulates intracellular O-glcNAcylation levels. J Am Chem Soc. 2006;128:16484–5. doi: 10.1021/ja066743n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Whitworth GE, Macauley MS, Stubbs KA, Dennis RJ, Taylor EJ, Davies GJ, et al. Analysis of PUGNAc and NAG-thiazoline as transition state analogues for human O-GlcNAcase: mechanistic and structural insights into inhibitor selectivity and transition state poise. J Am Chem Soc. 2007;129:635–44. doi: 10.1021/ja065697o. [DOI] [PubMed] [Google Scholar]
- 102.Zhu X, Zou L, Marsh SA, Marchase RB, Chatham JC. Inhibition of STIM1 Oligomerization by Protein O-Linked N-Acetylglucosamine: A Novel Metabolically Mediated Regulation of Cardiomyocyte Calcium Overload. Circulation. 2010;122 [Google Scholar]
- 103.Yuzwa SA, Macauley MS, Heinonen JE, Shan X, Dennis RJ, He Y, et al. A potent mechanism-inspired O-GlcNAcase inhibitor that blocks phosphorylation of tau in vivo. Nat Chem Biol. 2008;4:483–90. doi: 10.1038/nchembio.96. [DOI] [PubMed] [Google Scholar]
- 104.Watson LJ, Facundo HT, Ngoh GA, Ameen M, Brainard RE, Lemma KM, et al. O-linked beta-N-acetylglucosamine transferase is indispensable in the failing heart. Proc Natl Acad Sci U S A. 2010;107:17797–802. doi: 10.1073/pnas.1001907107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gross BJ, Kraybill BC, Walker S. Discovery of O-GlcNAc transferase inhibitors. J Am Chem Soc. 2005;127:14588–9. doi: 10.1021/ja0555217. [DOI] [PubMed] [Google Scholar]
- 106.Dehennaut V, Lefebvre T, Sellier C, Leroy Y, Gross B, Walker S, et al. O-linked N-acetylglucosaminyltransferase inhibition prevents G2/M transition in Xenopus laevis oocytes. J Biol Chem. 2007;282:12527–36. doi: 10.1074/jbc.M700444200. [DOI] [PubMed] [Google Scholar]
- 107.Gloster TM, Zandberg WF, Heinonen JE, Shen DL, Deng L, Vocadlo DJ. Hijacking a biosynthetic pathway yields a glycosyltransferase inhibitor within cells. Nat Chem Biol. 2011;7:174–81. doi: 10.1038/nchembio.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Klein AL, Berkaw MN, Buse MG, Ball LE. O-linked N-acetylglucosamine modification of insulin receptor substrate-1 occurs in close proximity to multiple SH2 domain binding motifs. Mol Cell Proteomics. 2009;8:2733–45. doi: 10.1074/mcp.M900207-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Teo CF, Ingale S, Wolfert MA, Elsayed GA, Not LG, Chatham JC, et al. Glycopeptide-specific monoclonal antibodies suggest new roles for O-GlcNAc. Nat Chem Biol. 2010;6:338–43. doi: 10.1038/nchembio.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shin SH, Love DC, Hanover JA. Elevated O-GlcNAc-dependent signaling through inducible mOGT expression selectively triggers apoptosis. Amino Acids. 2011;40:885–93. doi: 10.1007/s00726-010-0719-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Khidekel N, Arndt S, Lamarre-Vincent N, Lippert A, Poulin-Kerstien KG, Ramakrishnan B, et al. A chemoenzymatic approach toward the rapid and sensitive detection of O-GlcNAc posttranslational modifications. J Am Chem Soc. 2003;125:16162–3. doi: 10.1021/ja038545r. [DOI] [PubMed] [Google Scholar]
- 112.Kolb HC, Finn MG, Sharpless KB. Click Chemistry: Diverse Chemical Function from a Few Good Reactions. Angew Chem Int Ed Engl. 2001;40:2004–21. doi: 10.1002/1521-3773(20010601)40:11<2004::AID-ANIE2004>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 113.Gurcel C, Vercoutter-Edouart AS, Fonbonne C, Mortuaire M, Salvador A, Michalski JC, et al. Identification of new O-GlcNAc modified proteins using a click-chemistry-based tagging. Anal Bioanal Chem. 2008;390:2089–97. doi: 10.1007/s00216-008-1950-y. [DOI] [PubMed] [Google Scholar]
- 114.Hang HC, Yu C, Kato DL, Bertozzi CR. A metabolic labeling approach toward proteomic analysis of mucin-type O-linked glycosylation. Proc Natl Acad Sci U S A. 2003;100:14846–51. doi: 10.1073/pnas.2335201100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Boyce M, Carrico IS, Ganguli AS, Yu SH, Hangauer MJ, Hubbard SC, et al. Metabolic cross-talk allows labeling of O-linked beta-N-acetylglucosamine-modified proteins via the N-acetylgalactosamine salvage pathway. Proc Natl Acad Sci U S A. 2011;108:3141–6. doi: 10.1073/pnas.1010045108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Nandi A, Sprung R, Barma DK, Zhao Y, Kim SC, Falck JR. Global identification of O-GlcNAc-modified proteins. Anal Chem. 2006;78:452–8. doi: 10.1021/ac051207j. [DOI] [PubMed] [Google Scholar]
- 117.Vocadlo DJ, Hang HC, Kim EJ, Hanover JA, Bertozzi CR. A chemical approach for identifying O-GlcNAc-modified proteins in cells. Proc Natl Acad Sci U S A. 2003;100:9116–21. doi: 10.1073/pnas.1632821100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zaro BW, Yang YY, Hang HC, Pratt MR. Chemical reporters for fluorescent detection and identification of O-GlcNAc-modified proteins reveal glycosylation of the ubiquitin ligase NEDD4-1. Proc Natl Acad Sci U S A. 2011;108:8146–51. doi: 10.1073/pnas.1102458108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rexach JE, Rogers CJ, Yu SH, Tao J, Sun YE, Hsieh-Wilson LC. Quantification of O-glycosylation stoichiometry and dynamics using resolvable mass tags. Nat Chem Biol. 2010;6:645–51. doi: 10.1038/nchembio.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mikesh LM, Ueberheide B, Chi A, Coon JJ, Syka JE, Shabanowitz J, et al. The utility of ETD mass spectrometry in proteomic analysis. Biochim Biophys Acta. 2006;1764:1811–22. doi: 10.1016/j.bbapap.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Darula Z, Chalkley RJ, Baker P, Burlingame AL, Medzihradszky KF. Mass spectrometric analysis, automated identification and complete annotation of O-linked glycopeptides. Eur J Mass Spectrom (Chichester, Eng) 2010;16:421–8. doi: 10.1255/ejms.1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Deutsch EW, Shteynberg D, Lam H, Sun Z, Eng JK, Carapito C, et al. Trans-Proteomic Pipeline supports and improves analysis of electron transfer dissociation data sets. Proteomics. 2010;10:1190–5. doi: 10.1002/pmic.200900567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Vosseller K, Trinidad JC, Chalkley RJ, Specht CG, Thalhammer A, Lynn AJ, et al. O-linked N-acetylglucosamine proteomics of postsynaptic density preparations using lectin weak affinity chromatography and mass spectrometry. Mol Cell Proteomics. 2006;5:923–34. doi: 10.1074/mcp.T500040-MCP200. [DOI] [PubMed] [Google Scholar]
- 124.Chalkley RJ, Thalhammer A, Schoepfer R, Burlingame AL. Identification of protein O-GlcNAcylation sites using electron transfer dissociation mass spectrometry on native peptides. Proc Natl Acad Sci U S A. 2009;106:8894–9. doi: 10.1073/pnas.0900288106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wang Z, Udeshi ND, O'Malley M, Shabanowitz J, Hunt DF, Hart GW. Enrichment and site mapping of O-linked N-acetylglucosamine by a combination of chemical/enzymatic tagging, photochemical cleavage, and electron transfer dissociation mass spectrometry. Mol Cell Proteomics. 2010;9:153–60. doi: 10.1074/mcp.M900268-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Skorobogatko YV, Deuso J, Adolf-Bergfoyle J, Nowak MG, Gong Y, Lippa CF, et al. Human Alzheimer's disease synaptic O-GlcNAc site mapping and iTRAQ expression proteomics with ion trap mass spectrometry. Amino Acids. 2011;40:765–79. doi: 10.1007/s00726-010-0645-9. [DOI] [PubMed] [Google Scholar]
- 127.Wang Z, Park K, Comer F, Hsieh-Wilson LC, Saudek CD, Hart GW. Site-specific GlcNAcylation of human erythrocyte proteins: potential biomarker(s) for diabetes. Diabetes. 2009;58:309–17. doi: 10.2337/db08-0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Myers SA, Panning B, Burlingame AL. Polycomb repressive complex 2 is necessary for the normal site-specific O-GlcNAc distribution in mouse embryonic stem cells. Proc Natl Acad Sci U S A. 2011;108:9490–5. doi: 10.1073/pnas.1019289108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wang Z, Udeshi ND, Slawson C, Compton PD, Sakabe K, Cheung WD, et al. Extensive crosstalk between O-GlcNAcylation and phosphorylation regulates cytokinesis. Sci Signal. 2010;3:ra2. doi: 10.1126/scisignal.2000526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hornbeck PV, Chabra I, Kornhauser JM, Skrzypek E, Zhang B. PhosphoSite: A bioinformatics resource dedicated to physiological protein phosphorylation. Proteomics. 2004;4:1551–61. doi: 10.1002/pmic.200300772. [DOI] [PubMed] [Google Scholar]
- 131.Wang J, Torii M, Liu H, Hart GW, Hu ZZ. dbOGAP - an integrated bioinformatics resource for protein O-GlcNAcylation. BMC Bioinformatics. 2011;12:91. doi: 10.1186/1471-2105-12-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.McClain DA. Hexosamines as mediators of nutrient sensing and regulation in diabetes. J Diabetes Complications. 2002;16:72–80. doi: 10.1016/s1056-8727(01)00188-x. [DOI] [PubMed] [Google Scholar]
- 133.Virkamaki A, Daniels MC, Hamalainen S, Utriainen T, McClain D, Yki-Jarvinen H. Activation of the hexosamine pathway by glucosamine in vivo induces insulin resistance in multiple insulin sensitive tissues. Endocrinology. 1997;138:2501–7. doi: 10.1210/endo.138.6.5172. [DOI] [PubMed] [Google Scholar]
- 134.Patti ME, Virkamaki A, Landaker EJ, Kahn CR, Yki-Jarvinen H. Activation of the hexosamine pathway by glucosamine in vivo induces insulin resistance of early postreceptor insulin signaling events in skeletal muscle. Diabetes. 1999;48:1562–71. doi: 10.2337/diabetes.48.8.1562. [DOI] [PubMed] [Google Scholar]
- 135.Cooksey RC, McClain DA. Transgenic mice overexpressing the rate-limiting enzyme for hexosamine synthesis in skeletal muscle or adipose tissue exhibit total body insulin resistance. Ann N Y Acad Sci. 2002;967:102–11. doi: 10.1111/j.1749-6632.2002.tb04268.x. [DOI] [PubMed] [Google Scholar]
- 136.Hebert LF, Daniels MC, Zhou J, Crook ED, Turner RL, Simmons ST, et al. Overexpression of glutamine:fructose-6-phosphate amidotransferase in transgenic mice leads to insulin resistance. J Clin Invest. 1996;98:930–6. doi: 10.1172/JCI118876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Park SY, Ryu J, Lee W. O-GlcNAc modification on IRS-1 and Akt2 by PUGNAc inhibits their phosphorylation and induces insulin resistance in rat primary adipocytes. Exp Mol Med. 2005;37:220–9. doi: 10.1038/emm.2005.30. [DOI] [PubMed] [Google Scholar]
- 138.Robinson KA, Ball LE, Buse MG. Reduction of O-GlcNAc protein modification does not prevent insulin resistance in 3T3-L1 adipocytes. Am J Physiol Endocrinol Metab. 2007;292:E884–90. doi: 10.1152/ajpendo.00569.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chen G, Liu P, Thurmond DC, Elmendorf JS. Glucosamine-induced insulin resistance is coupled to O-linked glycosylation of Munc18c. FEBS letters. 2003;534:54–60. doi: 10.1016/s0014-5793(02)03774-2. [DOI] [PubMed] [Google Scholar]
- 140.Luo B, Parker GJ, Cooksey RC, Soesanto Y, Evans M, Jones D, et al. Chronic hexosamine flux stimulates fatty acid oxidation by activating AMP-activated protein kinase in adipocytes. J Biol Chem. 2007;282:7172–80. doi: 10.1074/jbc.M607362200. [DOI] [PubMed] [Google Scholar]
- 141.Comb DG, Roseman S. Glucosamine metabolism. IV. Glucosamine-6-phosphate deaminase. J Biol Chem. 1958;232:807–27. [PubMed] [Google Scholar]
- 142.Arreola R, Valderrama B, Morante ML, Horjales E. Two mammalian glucosamine-6-phosphate deaminases: a structural and genetic study. FEBS Lett. 2003;551:63–70. doi: 10.1016/s0014-5793(03)00896-2. [DOI] [PubMed] [Google Scholar]
- 143.Bonen A, Han XX, Tandon NN, Glatz JF, Lally J, Snook LA, et al. FAT/CD36 expression is not ablated in spontaneously hypertensive rats. J Lipid Res. 2009;50:740–8. doi: 10.1194/jlr.M800237-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Labarthe F, Khairallah M, Bouchard B, Stanley WC, Des Rosiers C. Fatty acid oxidation and its impact on response of spontaneously hypertensive rat hearts to an adrenergic stress: benefits of a medium-chain fatty acid. Am J Physiol Heart Circ Physiol. 2005;288:H1425–36. doi: 10.1152/ajpheart.00722.2004. [DOI] [PubMed] [Google Scholar]
- 145.Lauzier B, Merlen C, Vaillant F, McDuff J, Bouchard B, Beguin PC, et al. Post-translational modifications, a key process in CD36 function: Lessons from the spontaneously hypertensive rat heart. J Mol Cell Cardiol. 2011;51:99–108. doi: 10.1016/j.yjmcc.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 146.Lauzier B, Vaillant F, Bouchard B, Legault JT, Dolinsky VW, Gelinas R, et al. Glutamine modulates fatty acid metabolism in ex vivo working rat hearts via the hexosamine biosynthetic pathway. FASEB J. 2011;25:722–9. [Google Scholar]
- 147.Chatham JC, Laczy B, Durgan D, Young ME. Direct interrelationship between protein O-GlcNAcation and the cardiomyocyte circadian clock. Circ Res. 2009;105:e50. [Google Scholar]
- 148.Durgan DJ, Young ME. The cardiomyocyte circadian clock: emerging roles in health and disease. Circulation research. 2010;106:647–58. doi: 10.1161/CIRCRESAHA.109.209957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ngoh GA, Jones SP. O-GlcNAc signaling attenuates mitochondrial membrane permeability transition in cell death. Faseb J. 2008;22:1130. [Google Scholar]
- 150.Tsujimoto Y, Shimizu S. VDAC regulation by the Bcl-2 family of proteins. Cell Death Differ. 2000;7:1174–81. doi: 10.1038/sj.cdd.4400780. [DOI] [PubMed] [Google Scholar]
- 151.Tsujimoto Y, Shimizu S. Role of the mitochondrial membrane permeability transition in cell death. Apoptosis. 2007;12:835–40. doi: 10.1007/s10495-006-0525-7. [DOI] [PubMed] [Google Scholar]
- 152.Halestrap AP. What is the mitochondrial permeability transition pore? J Mol Cell Cardiol. 2009;46:821–31. doi: 10.1016/j.yjmcc.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 153.Hirschberg CB, Robbins PW, Abeijon C. Transporters of nucleotide sugars, ATP, and nucleotide sulfate in the endoplasmic reticulum and Golgi apparatus. Annu Rev Biochem. 1998;67:49–69. doi: 10.1146/annurev.biochem.67.1.49. [DOI] [PubMed] [Google Scholar]
- 154.Gerardy-Schahn R, Oelmann S, Bakker H. Nucleotide sugar transporters: biological and functional aspects. Biochimie. 2001;83:775–82. doi: 10.1016/s0300-9084(01)01322-0. [DOI] [PubMed] [Google Scholar]
- 155.Murphy E, Steenbergen C. Mechanisms underlying acute protection from cardiac ischemia-reperfusion injury. Physiol Rev. 2008;88:581–609. doi: 10.1152/physrev.00024.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Juhaszova M, Zorov DB, Yaniv Y, Nuss HB, Wang S, Sollott SJ. Role of glycogen synthase kinase-3beta in cardioprotection. Circ Res. 2009;104:1240–52. doi: 10.1161/CIRCRESAHA.109.197996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Zorov DB, Juhaszova M, Yaniv Y, Nuss HB, Wang S, Sollott SJ. Regulation and pharmacology of the mitochondrial permeability transition pore. Cardiovasc Res. 2009;83:213–25. doi: 10.1093/cvr/cvp151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gutierrez J, Ballinger SW, Darley-Usmar VM, Landar A. Free radicals, mitochondria, and oxidized lipids: the emerging role in signal transduction in vascular cells. Circ Res. 2006;99:924–32. doi: 10.1161/01.RES.0000248212.86638.e9. [DOI] [PubMed] [Google Scholar]
- 159.Landar A, Darley-Usmar VM. Nitric oxide and cell signaling: modulation of redox tone and protein modification. Amino Acids. 2003;25:313–21. doi: 10.1007/s00726-003-0019-7. [DOI] [PubMed] [Google Scholar]
- 160.Housley MP, Rodgers JT, Udeshi ND, Kelly TJ, Shabanowitz J, Hunt DF, et al. O-GlcNAc regulates FoxO activation in response to glucose. J Biol Chem. 2008;283:16283–92. doi: 10.1074/jbc.M802240200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Krebs EG. Protein-Phosphorylation and Cellular-Regulation.1. (Nobel Lecture) Angew Chem Int Edit. 1993;32:1122–9. doi: 10.1007/BF01149958. [DOI] [PubMed] [Google Scholar]