Chloroquine (original) (raw)
From Wikipedia, the free encyclopedia
Medication used to treat malaria
Pharmaceutical compound
Chloroquine
 |
|
|---|---|
 |
|
| Clinical data | |
| Pronunciation | |
| Trade names | Aralen, other |
| Other names | Chloroquine phosphate |
| AHFS/Drugs.com | Monograph |
| License data | US DailyMed: Chloroquine |
| Routes of administration | By mouth |
| ATC code | P01BA01 (WHO) P01BB52 (WHO) |
| Legal status | |
| Legal status | UK: P (Pharmacy medicines) US: ℞-only In general: ℞ (Prescription only) |
| Pharmacokinetic data | |
| Metabolism | Liver |
| Elimination half-life | 1-2 months |
| Identifiers | |
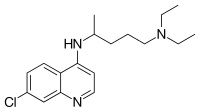
| IUPAC name (RS)-_N'_-(7-chloroquinolin-4-yl)-N,_N_-diethylpentane-1,4-diamine | |
| CAS Number | 54-05-7  Y Y |
| PubChem CID | 2719 |
| IUPHAR/BPS | 5535 |
| DrugBank | DB00608  Y Y |
| ChemSpider | 2618  Y Y |
| UNII | 886U3H6UFF |
| KEGG | D02366  Y Y |
| ChEBI | CHEBI:3638  Y Y |
| ChEMBL | ChEMBL76  Y Y |
| NIAID ChemDB | 000733 |
| CompTox Dashboard (EPA) | DTXSID2040446 |
| ECHA InfoCard | 100.000.175 |
| Chemical and physical data | |
| Formula | C18H26ClN3 |
| Molar mass | 319.88 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| SMILES Clc1cc2nccc(c2cc1)NC(C)CCCN(CC)CC | |
InChI InChI=1S/C18H26ClN3/c1-4-22(5-2)12-6-7-14(3)21-17-10-11-20-18-13-15(19)8-9-16(17)18/h8-11,13-14H,4-7,12H2,1-3H3,(H,20,21)  YKey:WHTVZRBIWZFKQO-UHFFFAOYSA-N YKey:WHTVZRBIWZFKQO-UHFFFAOYSA-N  Y Y |
|
| (verify) |
Chloroquine is an antiparasitic medication that treats malaria. It works by increasing the levels of haeme in the blood, a substance toxic to the malarial parasite. This kills the parasite and stops the infection from spreading.[1] Certain types of malaria, resistant strains, and complicated cases typically require different or additional medication.[1] Chloroquine is also occasionally used for amebiasis that is occurring outside the intestines, rheumatoid arthritis, and lupus erythematosus. [1] While it has not been formally studied in pregnancy, it appears safe.[1][2] It was studied to treat COVID-19 early in the pandemic, but these studies were largely halted in the summer of 2020, and the NIH does not recommend its use for this purpose.[3] It is taken by mouth.[1]
Common side effects include muscle problems, loss of appetite, diarrhea, and skin rash.[1] Serious side effects include problems with vision, muscle damage, seizures, and low blood cell levels.[1][4] Chloroquine is a member of the drug class 4-aminoquinoline.[1] As an antimalarial, it works against the asexual form of the malaria parasite in the stage of its life cycle within the red blood cell.[1] How it works in rheumatoid arthritis and lupus erythematosus is unclear.[1]
Chloroquine was discovered in 1934 by Hans Andersag.[5][6] It is on the World Health Organization's List of Essential Medicines.[7] It is available as a generic medication.[1]
Distribution of malaria in the world:[8]
o Elevated occurrence of chloroquine- or multi-resistant malaria
o Occurrence of chloroquine-resistant malaria
o No Plasmodium falciparum or chloroquine-resistance
o No malaria
Chloroquine has been used in the treatment and prevention of malaria from Plasmodium vivax, P. ovale, and P. malariae. It is generally not used for Plasmodium falciparum as there is widespread resistance to it.[9][10]
Chloroquine has been extensively used in mass drug administrations, which may have contributed to the emergence and spread of resistance. It is recommended to check if chloroquine is still effective in the region prior to using it.[11] In areas where resistance is present, other antimalarials, such as mefloquine or atovaquone, may be used instead. The Centers for Disease Control and Prevention recommend against treatment of malaria with chloroquine alone due to more effective combinations.[12]
In treatment of amoebic liver abscess, chloroquine may be used instead of or in addition to other medications in the event of failure of improvement with metronidazole or another nitroimidazole within five days or intolerance to metronidazole or a nitroimidazole.[13]
As it mildly suppresses the immune system, chloroquine is used in some autoimmune disorders, such as rheumatoid arthritis and has an off-label indication for lupus erythematosus.[1]
Side effects include blurred vision, nausea, vomiting, abdominal cramps, headache, diarrhea, swelling legs/ankles, shortness of breath, pale lips/nails/skin, muscle weakness, easy bruising/bleeding, hearing and mental problems.[14][15]
- Unwanted/uncontrolled movements (including tongue and face twitching, diskenesia, and dystonia)[14][16]
- Deafness or tinnitus[14]
- Nausea, vomiting, diarrhea, abdominal cramps[15]
- Headache[14]
- Mental/mood changes (such as confusion, personality changes, unusual thoughts/behavior, depression, feeling being watched, hallucinating)[14][15]
- Signs of serious infection (such as high fever, severe chills, persistent sore throat)[14]
- Skin itchiness, skin color changes, hair loss, and skin rashes[15][17]
- Chloroquine-induced itching is very common among black Africans (70%), but much less common in other races. It increases with age, and is so severe as to stop compliance with drug therapy. It is increased during malaria fever; its severity is correlated to the malaria parasite load in blood. Some evidence indicates it has a genetic basis and is related to chloroquine action with opiate receptors centrally or peripherally.[18]
- Triggering of a severe psoriasis attack in those with psoriasis[16]
- Unpleasant metallic taste
- This could be avoided by "taste-masked and controlled release" formulations such as multiple emulsions.[19]
- Chloroquine retinopathy (irreversible retinal damage)[16]
- Electrocardiographic changes[20]
- This manifests itself as either conduction disturbances (bundle-branch block, atrioventricular block) or cardiomyopathy — often with hypertrophy, restrictive physiology, and congestive heart failure. The changes may be irreversible. Only two cases have been reported requiring heart transplantation, suggesting this particular risk is very low. Electron microscopy of cardiac biopsies show pathognomonic cytoplasmic inclusion bodies.
- Pancytopenia, aplastic anemia, reversible agranulocytosis, low blood platelets, neutropenia[16]
- Worsening of the condition for those with porphyria[16]
- Delayed hypersensitivity syndrome has been described.[21]
Chloroquine has not been shown to have any harmful effects on the fetus when used in the recommended doses for malarial prophylaxis.[22] Small amounts of chloroquine are excreted in the breast milk of lactating women. However, this drug can be safely prescribed to infants, the effects are not harmful. Studies with mice show that radioactively tagged chloroquine passed through the placenta rapidly and accumulated in the fetal eyes which remained present five months after the drug was cleared from the rest of the body.[16][23] Women who are pregnant or planning on getting pregnant are still advised against traveling to malaria-risk regions.[22]
There is not enough evidence to determine whether chloroquine is safe to be given to people aged 65 and older. Since it is cleared by the kidneys, toxicity should be monitored carefully in people with poor kidney functions, as is more likely to be the case in the elderly.[16]
Chloroquine has a number of drug–drug interactions that might be of clinical concern:[_citation needed_]
- Ampicillin – levels may be reduced by chloroquine;[16]
- Antacids – may reduce absorption of chloroquine;[16]
- Cimetidine – may inhibit metabolism of chloroquine; increasing levels of chloroquine in the body;[16]
- Cyclosporine – levels may be increased by chloroquine;[16] and
- Mefloquine – may increase risk of convulsions.[16]
Chloroquine, in overdose, has a risk of death of about 20%.[24] It is rapidly absorbed from the gut with an onset of symptoms generally within an hour.[25] Symptoms of overdose may include sleepiness, vision changes, seizures, stopping of breathing, and heart problems such as ventricular fibrillation and low blood pressure.[24][25] Low blood potassium may also occur.[24]
While the usual dose of chloroquine used in treatment is 10 mg/kg, toxicity begins to occur at 20 mg/kg, and death may occur at 30 mg/kg.[24] In children as little as a single tablet can be fatal.[25][16]
Treatment recommendations include early mechanical ventilation, cardiac monitoring, and activated charcoal.[24] Intravenous fluids and vasopressors may be required with epinephrine being the vasopressor of choice.[24] Seizures may be treated with benzodiazepines.[24] Intravenous potassium chloride may be required, however this may result in high blood potassium later in the course of the disease.[24] Dialysis has not been found to be useful.[24]
Absorption of chloroquine is rapid and primarily happens in the gastrointestinal tract.[26] It is widely distributed in body tissues.[27] Protein binding in plasma ranges from 46% to 79%.[28] Its metabolism is partially hepatic, giving rise to its main metabolite, desethylchloroquine.[29] Its excretion is ≥50% as unchanged drug in urine, where acidification of urine increases its elimination.[_citation needed_] It has a very high volume of distribution, as it diffuses into the body's adipose tissue.[_citation needed_]
Accumulation of the drug may result in deposits that can lead to blurred vision and blindness.[30] It and related quinines have been associated with cases of retinal toxicity, particularly when provided at higher doses for longer times.[_citation needed_] With long-term doses, routine visits to an ophthalmologist are recommended.[_citation needed_]
Chloroquine is also a lysosomotropic agent, meaning it accumulates preferentially in the lysosomes of cells in the body.[_citation needed_] The pKa for the quinoline nitrogen of chloroquine is 8.5, meaning it is about 10% deprotonated at physiological pH (per the Henderson-Hasselbalch equation).[_citation needed_] This decreases to about 0.2% at a lysosomal pH of 4.6.[_citation needed_] Because the deprotonated form is more membrane-permeable than the protonated form, a quantitative "trapping" of the compound in lysosomes results.[_citation needed_]
Mechanism of action
[edit]
Medical quinolines
Hemozoin formation in P. falciparum: many antimalarials are strong inhibitors of hemozoin crystal growth.
The lysosomotropic character of chloroquine is believed to account for much of its antimalarial activity; the drug concentrates in the acidic food vacuole of the parasite and interferes with essential processes. Its lysosomotropic properties further allow for its use for in vitro experiments pertaining to intracellular lipid related diseases,[31][32] autophagy, and apoptosis.[33]
Inside red blood cells, the malarial parasite, which is then in its asexual lifecycle stage, must degrade hemoglobin to acquire essential amino acids, which the parasite requires to construct its own protein and for energy metabolism. Digestion is carried out in a vacuole of the parasitic cell.[_citation needed_]
Hemoglobin is composed of a protein unit (digested by the parasite) and a heme unit (not used by the parasite). During this process, the parasite releases the toxic and soluble molecule heme. The heme moiety consists of a porphyrin ring called Fe(II)-protoporphyrin IX (FP). To avoid destruction by this molecule, the parasite biocrystallizes heme to form hemozoin, a nontoxic molecule. Hemozoin collects in the digestive vacuole as insoluble crystals.[_citation needed_]
Chloroquine enters the red blood cell by simple diffusion, inhibiting the parasite cell and digestive vacuole. Chloroquine (CQ) then becomes protonated (to CQ2+), as the digestive vacuole is known to be acidic (pH 4.7); chloroquine then cannot leave by diffusion. Chloroquine caps hemozoin molecules to prevent further biocrystallization of heme, thus leading to heme buildup. Chloroquine binds to heme (or FP) to form the FP-chloroquine complex; this complex is highly toxic to the cell and disrupts membrane function. Action of the toxic FP-chloroquine and FP results in cell lysis and ultimately parasite cell autodigestion.[34] Parasites that do not form hemozoin are therefore resistant to chloroquine.[35]
Resistance in malaria
[edit]
Since the first documentation of P. falciparum chloroquine resistance in the 1950s, resistant strains have appeared throughout East and West Africa, Southeast Asia, and South America. The effectiveness of chloroquine against P. falciparum has declined as resistant strains of the parasite evolved.
Resistant parasites are able to rapidly remove chloroquine from the digestive vacuole using a transmembrane pump. Chloroquine-resistant parasites pump chloroquine out at 40 times the rate of chloroquine-sensitive parasites; the pump is coded by the P. falciparum chloroquine resistance transporter (PfCRT) gene.[36] The natural function of the chloroquine pump is to transport peptides: mutations to the pump that allow it to pump chloroquine out impairs its function as a peptide pump and comes at a cost to the parasite, making it less fit.[37]
Resistant parasites also frequently have mutation in the ABC transporter P. falciparum multidrug resistance (PfMDR1) gene, although these mutations are thought to be of secondary importance compared to PfCRT. An altered chloroquine-transporter protein, CG2 has been associated with chloroquine resistance, but other mechanisms of resistance also appear to be involved.[38]
Verapamil, a Ca2+ channel blocker, has been found to restore both the chloroquine concentration ability and sensitivity to this drug. Other agents which have been shown to reverse chloroquine resistance in malaria are chlorpheniramine, gefitinib, imatinib, tariquidar and zosuquidar.[39]
As of 2014[update] chloroquine is still effective against poultry malaria in Thailand. Sohsuebngarm et al. 2014 test P. gallinaceum at Chulalongkorn University and find the parasite is not resistant.[40]: 1237 Sertraline, fluoxetine and paroxetine reverse chloroquine resistance, making resistant biotypes susceptible if used in a cotreatment.[41]
Chloroquine has antiviral effects against some viruses.[42] It increases late endosomal and lysosomal pH, resulting in impaired release of the virus from the endosome or lysosome — release of the virus requires a low pH. The virus is therefore unable to release its genetic material into the cell and replicate.[43][44]
Chloroquine also seems to act as a zinc ionophore that allows extracellular zinc to enter the cell and inhibit viral RNA-dependent RNA polymerase.[45][46]
Chloroquine inhibits thiamine uptake.[47] It acts specifically on the transporter SLC19A3.
Against rheumatoid arthritis, it operates by inhibiting lymphocyte proliferation, phospholipase A2, antigen presentation in dendritic cells, release of enzymes from lysosomes, release of reactive oxygen species from macrophages, and production of IL-1.[_medical citation needed_]
In Peru, the indigenous people extracted the bark of the Cinchona tree (Cinchona officinalis)[48] and used the extract to fight chills and fever in the seventeenth century. In 1633, this herbal medicine was introduced in Europe, where it was given the same use and also began to be used against malaria. The quinoline antimalarial drug quinine was isolated from the extract in 1820.[49]: 130–131
3-Methylchloroquine (sontochin)
After World War I, the German government sought alternatives to quinine. Chloroquine, a synthetic analogue with the same mechanism of action was discovered in 1934, by Hans Andersag and coworkers at the Bayer laboratories, who named it resochin.[50][51] It was ignored for a decade, because it was considered too toxic for human use. Instead, in World War II, the German Africa Corps used the chloroquine analogue 3-methyl-chloroquine, known as sontochin. After Allied forces arrived in Tunis, sontochin fell into the hands of Americans, who sent the material back to the United States for analysis, leading to renewed interest in chloroquine.[52][53] United States government-sponsored clinical trials for antimalarial drug development showed unequivocally that chloroquine has a significant therapeutic value as an antimalarial drug.[49]: 61–66 It was introduced into clinical practice in 1947 for the prophylactic treatment of malaria.[54]
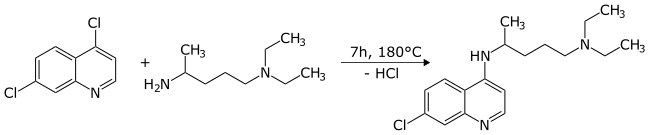
The first synthesis of chloroquine was disclosed in a patent filed by IG Farben in 1937.[55] In the final step, 4,7-dichloroquinoline was reacted with 1-diethylamino-4-aminopentane.
By 1949, chloroquine manufacturing processes had been established to allow its widespread use.[56]
Society and culture
[edit]
Resochin tablet package
Chloroquine comes in tablet form as the phosphate, sulfate, and hydrochloride salts. Chloroquine is usually dispensed as the phosphate.[57]
Brand names include Chloroquine FNA, Resochin, Dawaquin, and Lariago.[58]
Chloroquine, in various chemical forms, is used to treat and control surface growth of anemones and algae, and many protozoan infections in aquariums,[59] e.g. the fish parasite Amyloodinium ocellatum.[60] It is also used in poultry malaria.[40]: 1237
Chloroquine was proposed as a treatment for SARS, with in vitro tests inhibiting the severe acute respiratory syndrome coronavirus (SARS-CoV).[61][62] In October 2004, a published report stated that chloroquine acts as an effective inhibitor of the replication of SARS-CoV in vitro.[61] In August 2005, a peer-reviewed study confirmed and expanded upon the results.[63]
Chloroquine was being considered in 2003, in pre-clinical models as a potential agent against chikungunya fever.[64]
 |
This article needs to be updated. Please help update this article to reflect recent events or newly available information. (April 2024) |
|---|
A World Health Organization infographic that states that hydroxychloroquine does not prevent illness or death from COVID-19.
Chloroquine and hydroxychloroquine are anti-malarial medications also used against some auto-immune diseases.[65] Chloroquine, along with hydroxychloroquine, was an early experimental treatment for COVID-19.[66] Neither drug has been useful to prevent or treat SARS-CoV-2 infection.[67][68][69][70][71][72] Administration of chloroquine or hydroxychloroquine to COVID-19 patients, either as monotherapies or in conjunction with azithromycin, has been associated with deleterious outcomes, such as QT prolongation.[73][74] As of 2024,[update] scientific evidence does not substantiate the efficacy of hydroxychloroquine, with or without the addition of azithromycin, in the therapeutic management of COVID-19.[73][75]
Cleavage of the SARS-CoV-2 S2 spike protein required for viral entry into cells can be accomplished by proteases TMPRSS2 located on the cell membrane, or by cathepsins (primarily cathepsin L) in endolysosomes.[76] Hydroxychloroquine inhibits the action of cathepsin L in endolysosomes, but because cathepsin L cleavage is minor compared to TMPRSS2 cleavage, hydroxychloroquine does little to inhibit SARS-CoV-2 infection.[76]
Several countries initially used chloroquine or hydroxychloroquine for treatment of persons hospitalized with COVID-19 (as of March 2020), though the drug was not formally approved through clinical trials.[77][78] From April to June 2020, there was an emergency use authorization for their use in the United States,[79] and was used off label for potential treatment of the disease.[80] On 24 April 2020, citing the risk of "serious heart rhythm problems", the FDA posted a caution against using the drug for COVID-19 "outside of the hospital setting or a clinical trial".[81]
Their use was withdrawn as a possible treatment for COVID-19 infection when it proved to have no benefit for hospitalized patients with severe COVID-19 illness in the international Solidarity trial and UK RECOVERY Trial.[82][83] On 15 June 2020, the FDA revoked its emergency use authorization, stating that it was "no longer reasonable to believe" that the drug was effective against COVID-19 or that its benefits outweighed "known and potential risks".[84][85][86] In fall of 2020, the National Institutes of Health issued treatment guidelines recommending against the use of hydroxychloroquine for COVID-19 except as part of a clinical trial.[65]
In 2021, hydroxychloroquine was part of the recommended treatment for mild cases in India.[87]
In 2020, the speculative use of hydroxychloroquine for COVID-19 threatened its availability for people with established indications (malaria and auto-immune diseases).[69]
The radiosensitizing and chemosensitizing properties of chloroquine are being evaluated for anticancer strategies in humans.[88][89] In biomedicinal science, chloroquine is used for in vitro experiments to inhibit lysosomal degradation of protein products. Chloroquine and its modified forms have also been evaluated as treatment options for inflammatory conditions like rheumatoid arthritis and inflammatory bowel disease.[90]
- ^ a b c d e f g h i j k l "Aralen Phosphate". The American Society of Health-System Pharmacists. Archived from the original on 8 December 2015. Retrieved 2 December 2015.
- ^ "Chloroquine Use During Pregnancy". Drugs.com. Archived from the original on 16 April 2019. Retrieved 16 April 2019. There are no controlled data in human pregnancies.
- ^ "Chloroquine or Hydroxychloroquine". COVID-19 Treatment Guidelines. National Institutes of Health. Archived from the original on 28 August 2020. Retrieved 14 February 2021.
- ^ Mittra RA, Mieler WG (2013). "Chapter 89 – Drug Toxicity of the Posterior Segment". Retina (Fifth ed.). W.B. Saunders. pp. 1532–1554. doi:10.1016/B978-1-4557-0737-9.00089-8. ISBN 978-1-4557-0737-9. Retrieved 25 March 2020.
- ^ Manson P, Cooke G, Zumla A, eds. (2009). Manson's tropical diseases (22nd ed.). [Edinburgh]: Saunders. p. 1240. ISBN 978-1-4160-4470-3. Archived from the original on 2 November 2018. Retrieved 9 September 2017.
- ^ Bhattacharjee M (2016). Chemistry of Antibiotics and Related Drugs. Springer. p. 184. ISBN 978-3-319-40746-3. Archived from the original on 1 November 2018. Retrieved 9 September 2017.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06.
- ^ "Frequently Asked Questions (FAQs): If I get malaria, will I have it for the rest of my life?". US Centers for Disease Control and Prevention. 8 February 2010. Archived from the original on 13 May 2012. Retrieved 14 May 2012.
- ^ Plowe CV (2005). "Antimalarial drug resistance in Africa: strategies for monitoring and deterrence". Malaria: Drugs, Disease and Post-genomic Biology. Current Topics in Microbiology and Immunology. Vol. 295. Springer. pp. 55–79. doi:10.1007/3-540-29088-5_3. ISBN 3-540-25363-7. PMID 16265887.
- ^ Uhlemann AC, Krishna S (2005). "Antimalarial Multi-Drug Resistance in Asia: Mechanisms and Assessment". Malaria: Drugs, Disease and Post-genomic Biology. Current Topics in Microbiology and Immunology. Vol. 295. Springer. pp. 39–53. doi:10.1007/3-540-29088-5_2. ISBN 978-3-540-25363-1. PMID 16265886.
- ^ "Chloroquine phosphate tablet – chloroquine phosphate tablet, coated". dailymed.nlm.nih.gov. Archived from the original on 8 December 2015. Retrieved 4 November 2015.
- ^ CDC. Health information for international travel 2001–2002. Atlanta, Georgia: U.S. Department of Health and Human Services, Public Health Service, 2001.
- ^ Amebic Hepatic Abscesses~treatment at eMedicine
- ^ a b c d e f "Drugs & Medications". www.webmd.com. Retrieved 22 March 2020.
- ^ a b c d "Chloroquine Side Effects: Common, Severe, Long Term". Drugs.com. Retrieved 22 March 2020.
- ^ a b c d e f g h i j k l m "Chloroquine phosphate tablet". DailyMed. 8 October 2018. Retrieved 7 April 2020.
- ^ "Chloroquine: MedlinePlus Drug Information". medlineplus.gov. Retrieved 22 March 2020.
- ^ Ajayi AA (September 2000). "Mechanisms of chloroquine-induced pruritus". Clinical Pharmacology and Therapeutics. 68 (3): 336. PMID 11014416.
- ^ Vaziri A, Warburton B (1994). "Slow release of chloroquine phosphate from multiple taste-masked W/O/W multiple emulsions". Journal of Microencapsulation. 11 (6): 641–648. doi:10.3109/02652049409051114. PMID 7884629.
- ^ Tönnesmann E, Kandolf R, Lewalter T (June 2013). "Chloroquine cardiomyopathy - a review of the literature". Immunopharmacology and Immunotoxicology. 35 (3): 434–442. doi:10.3109/08923973.2013.780078. PMID 23635029. S2CID 37926477.
- ^ Kanny G, Renaudin JM, Lecompte T, Moneret-Vautrin DA (February 2002). "Chloroquine hypersensitivity syndrome". Eur J Intern Med. 13 (1): 75–76. doi:10.1016/s0953-6205(01)00195-9. PMID 11836088.
- ^ a b "Malaria – Chapter 3 – 2016 Yellow Book". wwwnc.cdc.gov. Archived from the original on 14 January 2016. Retrieved 11 November 2015.
- ^ Ullberg S, Lindquist NG, Sjòstrand SE (September 1970). "Accumulation of chorio-retinotoxic drugs in the foetal eye". Nature. 227 (5264): 1257–1258. Bibcode:1970Natur.227.1257U. doi:10.1038/2271257a0. PMID 5452818. S2CID 4191322.
- ^ a b c d e f g h i Ling Ngan Wong A, Tsz Fung Cheung I, Graham CA (February 2008). "Hydroxychloroquine overdose: case report and recommendations for management". European Journal of Emergency Medicine. 15 (1): 16–18. doi:10.1097/MEJ.0b013e3280adcb56. PMID 18180661. S2CID 41205035.
- ^ a b c Smith ER, Klein-Schwartz W (May 2005). "Are 1-2 dangerous? Chloroquine and hydroxychloroquine exposure in toddlers". The Journal of Emergency Medicine. 28 (4): 437–443. doi:10.1016/j.jemermed.2004.12.011. PMID 15837026.
- ^ "Chloroquine". §6.1 Absorption by route of exposure. Retrieved 24 April 2020.
- ^ Adelusi SA, Salako LA (November 1982). "Tissue and blood concentrations of chloroquine following chronic administration in the rat". The Journal of Pharmacy and Pharmacology. 34 (11): 733–735. doi:10.1111/j.2042-7158.1982.tb06211.x. PMID 6129306. S2CID 35269419.
- ^ Walker O, Birkett DJ, Alván G, Gustafsson LL, Sjöqvist F (March 1983). "Characterization of chloroquine plasma protein binding in man". British Journal of Clinical Pharmacology. 15 (3): 375–377. doi:10.1111/j.1365-2125.1983.tb01513.x. PMC 1427768. PMID 6849768.
- ^ Projean D, Baune B, Farinotti R, Flinois JP, Beaune P, Taburet AM, et al. (June 2003). "In vitro metabolism of chloroquine: identification of CYP2C8, CYP3A4, and CYP2D6 as the main isoforms catalyzing N-desethylchloroquine formation". Drug Metabolism and Disposition. 31 (6): 748–754. doi:10.1124/dmd.31.6.748. PMID 12756207. S2CID 2115928.
- ^ Handzel DM, Romanou-Papadopoulou V, Briesen S (September 2021). "[Visual loss under chloroquine treatment-and not (only) due to bull's eye maculopathy!]" [Visual loss under chloroquine treatment-and not (only) due to bull's eye maculopathy!]. Der Ophthalmologe (in German). 118 (9): 953–955. doi:10.1007/s00347-020-01288-y. PMID 33300096. S2CID 228089310.
- ^ Chen PM, Gombart ZJ, Chen JW (March 2011). "Chloroquine treatment of ARPE-19 cells leads to lysosome dilation and intracellular lipid accumulation: possible implications of lysosomal dysfunction in macular degeneration". Cell & Bioscience. 1 (1): 10. doi:10.1186/2045-3701-1-10. PMC 3125200. PMID 21711726.
- ^ Kurup P, Zhang Y, Xu J, Venkitaramani DV, Haroutunian V, Greengard P, et al. (April 2010). "Abeta-mediated NMDA receptor endocytosis in Alzheimer's disease involves ubiquitination of the tyrosine phosphatase STEP61". The Journal of Neuroscience. 30 (17): 5948–5957. doi:10.1523/JNEUROSCI.0157-10.2010. PMC 2868326. PMID 20427654.
- ^ Kim EL, Wüstenberg R, Rübsam A, Schmitz-Salue C, Warnecke G, Bücker EM, et al. (April 2010). "Chloroquine activates the p53 pathway and induces apoptosis in human glioma cells". Neuro-Oncology. 12 (4): 389–400. doi:10.1093/neuonc/nop046. PMC 2940600. PMID 20308316.
- ^ Hempelmann E (March 2007). "Hemozoin biocrystallization in Plasmodium falciparum and the antimalarial activity of crystallization inhibitors". Parasitology Research. 100 (4): 671–676. doi:10.1007/s00436-006-0313-x. PMID 17111179. S2CID 30446678.
- ^ Lin JW, Spaccapelo R, Schwarzer E, Sajid M, Annoura T, Deroost K, et al. (June 2015). "Replication of Plasmodium in reticulocytes can occur without hemozoin formation, resulting in chloroquine resistance" (PDF). The Journal of Experimental Medicine. 212 (6): 893–903. doi:10.1084/jem.20141731. PMC 4451122. PMID 25941254. Archived (PDF) from the original on 22 September 2017. Retrieved 4 November 2018.
- ^ Martin RE, Marchetti RV, Cowan AI, Howitt SM, Bröer S, Kirk K (September 2009). "Chloroquine transport via the malaria parasite's chloroquine resistance transporter". Science. 325 (5948): 1680–1682. Bibcode:2009Sci...325.1680M. doi:10.1126/science.1175667. PMID 19779197. S2CID 206520905.
- ^ Shafik SH, Cobbold SA, Barkat K, Richards SN, Lancaster NS, Llinás M, et al. (August 2020). "The natural function of the malaria parasite's chloroquine resistance transporter". Nature Communications. 11 (1): 3922. Bibcode:2020NatCo..11.3922S. doi:10.1038/s41467-020-17781-6. PMC 7413254. PMID 32764664.
- ^ Tripathi KD (2003). Essentials of Medical Pharmacology (fifth ed.). Jaypee Brothers Medical Publisher Ltd. pp. 739–740.
- ^ Alcantara LM, Kim J, Moraes CB, Franco CH, Franzoi KD, Lee S, et al. (June 2013). "Chemosensitization potential of P-glycoprotein inhibitors in malaria parasites". Experimental Parasitology. 134 (2): 235–243. doi:10.1016/j.exppara.2013.03.022. PMID 23541983.
- ^ a b McDougald LR, Cervantes HM, Jenkins MC, Hess M, Beckstead R (22 November 2019). "Protozoal Infections". Diseases of Poultry (14 ed.). Wiley. ISBN 9781119371199.
- ^ Munoz-Bellido JL, Munoz-Criado S, Garcìa-Rodrìguez JA (April 2000). "Antimicrobial activity of psychotropic drugs: selective serotonin reuptake inhibitors". International Journal of Antimicrobial Agents. 14 (3). International Society of Chemotherapy (Elsevier): 177–180. doi:10.1016/s0924-8579(99)00154-5. PMID 10773485.
- ^ Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R (November 2003). "Effects of chloroquine on viral infections: an old drug against today's diseases?". The Lancet. Infectious Diseases. 3 (11): 722–727. doi:10.1016/s1473-3099(03)00806-5. PMC 7128816. PMID 14592603.
- ^ Al-Bari MA (February 2017). "Targeting endosomal acidification by chloroquine analogs as a promising strategy for the treatment of emerging viral diseases". Pharmacology Research & Perspectives. 5 (1): e00293. doi:10.1002/prp2.293. PMC 5461643. PMID 28596841.
- ^ Fredericksen BL, Wei BL, Yao J, Luo T, Garcia JV (November 2002). "Inhibition of endosomal/lysosomal degradation increases the infectivity of human immunodeficiency virus". Journal of Virology. 76 (22): 11440–11446. doi:10.1128/JVI.76.22.11440-11446.2002. PMC 136743. PMID 12388705.
- ^ Xue J, Moyer A, Peng B, Wu J, Hannafon BN, Ding WQ (1 October 2014). "Chloroquine is a zinc ionophore". PLOS ONE. 9 (10): e109180. Bibcode:2014PLoSO...9j9180X. doi:10.1371/journal.pone.0109180. PMC 4182877. PMID 25271834.
- ^ te Velthuis AJ, van den Worm SH, Sims AC, Baric RS, Snijder EJ, van Hemert MJ (November 2010). "Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture". PLOS Pathogens. 6 (11): e1001176. doi:10.1371/journal.ppat.1001176. PMC 2973827. PMID 21079686.
- ^ Huang Z, Srinivasan S, Zhang J, Chen K, Li Y, Li W, et al. (2012). "Discovering thiamine transporters as targets of chloroquine using a novel functional genomics strategy". PLOS Genetics. 8 (11): e1003083. doi:10.1371/journal.pgen.1003083. PMC 3510038. PMID 23209439.
- ^ Fern K (2010–2020). "Cinchona officinalis – L." Plans for a Future. Archived from the original on 25 August 2017. Retrieved 2 February 2020.
- ^ a b Institute of Medicine (US) Committee on the Economics of Antimalarial Drug (2004). Arrow KJ, Panosian C, Gelband H (eds.). Saving lives, buying time : economics of malaria drugs in an age of resistance. National Academies Press. doi:10.17226/11017. ISBN 9780309092180. PMID 25009879.
- ^ Kouznetsov VV, Amado Torres DF (September 2008). "Antimalarials: construction of molecular hybrids based on chloroquine". Universitas Scientiarum. 13 (3): 306–320.
- ^ Krafts K, Hempelmann E, Skórska-Stania A (July 2012). "From methylene blue to chloroquine: a brief review of the development of an antimalarial therapy". Parasitology Research. 111 (1): 1–6. doi:10.1007/s00436-012-2886-x. PMID 22411634. S2CID 54526057.
- ^ Sneader W (2005). Drug Discovery. A History. Wiley. ISBN 0471899801.
- ^ Pou S, Winter RW, Nilsen A, Kelly JX, Li Y, Doggett JS, et al. (July 2012). "Sontochin as a guide to the development of drugs against chloroquine-resistant malaria". Antimicrobial Agents and Chemotherapy. 56 (7): 3475–3480. doi:10.1128/AAC.00100-12. PMC 3393441. PMID 22508305. S2CID 32186437.
- ^ "The History of Malaria, an Ancient Disease". Centers for Disease Control. 29 July 2019. Archived from the original on 28 August 2010.
- ^ DE patent 683692, Andersag, Hans; Breitner, Stefan & Jung, Heinrich, "Process for the preparation of quinoline compounds containing amino groups with basic substituents in the 4-position", issued 1939-11-13, assigned to IG Farbenindustrie AG
- ^ Kenyon RL, Wiesner JA, Kwartler CE (1 April 1949). "Chloroquine manufacture". Industrial & Engineering Chemistry. 41 (4): 654–662. doi:10.1021/ie50472a002.
- ^ "Chloroquine". nih.gov. National Institutes of Health. Retrieved 24 March 2020.
- ^ "Ipca Laboratories: Formulations – Branded". Archived from the original on 6 April 2019. Retrieved 14 March 2020.
- ^ Hemdal J (20 February 2013). "Aquarium Fish: Chloroquine: A "New" Drug for Treating Fish Diseases". Advanced Aquarist. Archived from the original on 15 March 2013. Retrieved 26 March 2020.
- ^ Francis-Floyd R, Floyd MR. "Amyloodinium ocellatum, an Important Parasite of Cultured Marine Fish" (PDF). agrilife.org. Archived from the original (PDF) on 1 June 2015. Retrieved 24 March 2020.
- ^ a b Keyaerts E, Vijgen L, Maes P, Neyts J, Van Ranst M (October 2004). "In vitro inhibition of severe acute respiratory syndrome coronavirus by chloroquine". Biochemical and Biophysical Research Communications. 323 (1): 264–268. doi:10.1016/j.bbrc.2004.08.085. PMC 7092815. PMID 15351731.
- ^ Devaux CA, Rolain JM, Colson P, Raoult D (May 2020). "New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19?". International Journal of Antimicrobial Agents. 55 (5): 105938. doi:10.1016/j.ijantimicag.2020.105938. PMC 7118659. PMID 32171740.
- ^ Vincent MJ, Bergeron E, Benjannet S, Erickson BR, Rollin PE, Ksiazek TG, et al. (August 2005). "Chloroquine is a potent inhibitor of SARS coronavirus infection and spread". Virology Journal. 2: 69. doi:10.1186/1743-422X-2-69. PMC 1232869. PMID 16115318.
- ^ Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R (November 2003). "Effects of chloroquine on viral infections: an old drug against today's diseases?". The Lancet. Infectious Diseases. 3 (11): 722–727. doi:10.1016/S1473-3099(03)00806-5. PMC 7128816. PMID 14592603.
- ^ a b "Chloroquine or Hydroxychloroquine". COVID-19 Treatment Guidelines. National Institutes of Health. Archived from the original on 28 August 2020. Retrieved 14 February 2021.
- ^ "Coronavirus (COVID-19) Update: Daily Roundup March 30, 2020". FDA. 30 March 2020. Archived from the original on 19 October 2020. Retrieved 28 February 2021.
- ^ Smit M, Marinosci A, Agoritsas T, Calmy A (April 2021). "Prophylaxis for COVID-19: a systematic review". Clinical Microbiology and Infection (Systematic review). 27 (4): 532–537. doi:10.1016/j.cmi.2021.01.013. PMC 7813508. PMID 33476807.
- ^ Meyerowitz EA, Vannier AG, Friesen MG, Schoenfeld S, Gelfand JA, Callahan MV, et al. (May 2020). "Rethinking the role of hydroxychloroquine in the treatment of COVID-19". FASEB Journal. 34 (5): 6027–6037. doi:10.1096/fj.202000919. PMC 7267640. PMID 32350928.
- ^ a b Juurlink DN (April 2020). "Safety considerations with chloroquine, hydroxychloroquine and azithromycin in the management of SARS-CoV-2 infection". CMAJ. 192 (17): E450–E453. doi:10.1503/cmaj.200528. PMC 7207200. PMID 32269021.
- ^ "Assessment of Evidence for COVID-19-Related Treatments: Updated 4/3/2020". American Society of Health-System Pharmacists. Archived from the original on 14 April 2021. Retrieved 7 April 2020.
- ^ Yazdany J, Kim AH (June 2020). "Use of Hydroxychloroquine and Chloroquine During the COVID-19 Pandemic: What Every Clinician Should Know". Annals of Internal Medicine. 172 (11): 754–755. doi:10.7326/M20-1334. PMC 7138336. PMID 32232419.
- ^ Singh B, Ryan H, Kredo T, Chaplin M, Fletcher T, et al. (Cochrane Infectious Diseases Group) (February 2021). "Chloroquine or hydroxychloroquine for prevention and treatment of COVID-19". The Cochrane Database of Systematic Reviews. 2021 (2): CD013587. doi:10.1002/14651858.CD013587.pub2. PMC 8094389. PMID 33624299.
- ^ a b Nag K, Tripura K, Datta A, Karmakar N, Singh M, Singh M, et al. (2024). "Effect of Hydroxychloroquine and Azithromycin Combination Use in COVID-19 Patients - An Umbrella Review". Indian J Community Med. 49 (1): 22–27. doi:10.4103/ijcm.ijcm_983_22. PMC 10900474. PMID 38425958.
- ^ Jankelson L, Karam G, Becker ML, Chinitz LA, Tsai M (2020). "QT prolongation, torsades de pointes, and sudden death with short courses of chloroquine or hydroxychloroquine as used in COVID-19: A systematic review". Heart Rhythm. 17 (9): 1472–1479. doi:10.1016/j.hrthm.2020.05.008. PMC 7211688. PMID 32438018.
- ^ Hong H, Friedland A, Hu M, Anstrom KJ, Halabi S, McKinnon JE, et al. (June 2023). "Safety and efficacy of hydroxychloroquine as prophylactic against COVID-19 in healthcare workers: a meta-analysis of randomised clinical trials". BMJ Open. 13 (6): e065305. doi:10.1136/bmjopen-2022-065305.
- ^ a b Jackson CB, Farzan M, Chen B, Choe H (January 2022). "Mechanisms of SARS-CoV-2 entry into cells". Nature Reviews. Molecular Cell Biology. 23 (1): 3–20. doi:10.1038/s41580-021-00418-x. PMC 8491763. PMID 34611326.
- ^ "Information for clinicians on therapeutic options for COVID-19 patients". US Centers for Disease Control and Prevention. 21 March 2020. Archived from the original on 8 April 2020. Retrieved 22 March 2020.
- ^ Hinton DM (28 March 2020). "Request for Emergency Use Authorization For Use of Chloroquine Phosphate or Hydroxychloroquine Sulfate Supplied From the Strategic National Stockpile for Treatment of 2019 Coronavirus Disease" (PDF). U.S. Food and Drug Administration (FDA). Archived from the original on 2 October 2020. Retrieved 30 March 2020.
- ^ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 8 April 2020. Retrieved 9 April 2020.
- ^ Kalil AC (May 2020). "Treating COVID-19-Off-Label Drug Use, Compassionate Use, and Randomized Clinical Trials During Pandemics". JAMA. 323 (19): 1897–1898. doi:10.1001/jama.2020.4742. PMID 32208486.
- ^ "FDA cautions against use of hydroxychloroquine or chloroquine for COVID-19 outside of the hospital setting or a clinical trial due to risk of heart rhythm problems". U.S. Food and Drug Administration (FDA). 24 April 2020. Archived from the original on 4 November 2020. Retrieved 28 February 2021.
- ^ Mulier T (17 June 2020). "Hydroxychloroquine halted in WHO-sponsored COVID-19 trials". Bloomberg. Archived from the original on 11 October 2020. Retrieved 17 June 2020.
- ^ "No clinical benefit from use of hydroxychloroquine in hospitalised patients with COVID-19". Recovery Trial, Nuffield Department of Population Health, University of Oxford, UK. 5 June 2020. Archived from the original on 8 October 2020. Retrieved 7 June 2020.
- ^ "Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Chloroquine and Hydroxychloroquine". U.S. Food and Drug Administration (FDA) (Press release). 15 June 2020. Archived from the original on 15 June 2020. Retrieved 15 June 2020.
- ^ Lovelace Jr B (15 June 2020). "FDA revokes emergency use of hydroxychloroquine". CNBC. Archived from the original on 11 October 2020. Retrieved 28 February 2021.
- ^ "Frequently Asked Questions on the Revocation of the Emergency Use Authorization for Hydroxychloroquine Sulfate and Chloroquine Phosphate" (PDF). U.S. Food and Drug Administration (FDA). 15 June 2020. Archived from the original on 15 April 2021. Retrieved 15 June 2020.
- ^ "Clinical Management Protocol for Covid-19 (in Adults)" (PDF). Ministry of Health and Family Welfare. 24 May 2021. Archived (PDF) from the original on 5 December 2021. Retrieved 30 November 2024. "Health ministry issues revised clinical management protocols for Covid-19 amid spurt in cases". Times of India. Press Trust of India. 13 June 2021. Archived from the original on 11 July 2021. Retrieved 10 July 2021.
- ^ Savarino A, Lucia MB, Giordano F, Cauda R (October 2006). "Risks and benefits of chloroquine use in anticancer strategies". The Lancet. Oncology. 7 (10): 792–793. doi:10.1016/S1470-2045(06)70875-0. PMID 17012039.
- ^ Sotelo J, Briceño E, López-González MA (March 2006). "Adding chloroquine to conventional treatment for glioblastoma multiforme: a randomized, double-blind, placebo-controlled trial". Annals of Internal Medicine. 144 (5): 337–343. doi:10.7326/0003-4819-144-5-200603070-00008. PMID 16520474. S2CID 24807955.
"Summaries for patients. Adding chloroquine to conventional chemotherapy and radiotherapy for glioblastoma multiforme". Annals of Internal Medicine. 144 (5): I31. March 2006. doi:10.7326/0003-4819-144-5-200603070-00004. PMID 16520470. - ^ Goel P, Gerriets V (January 2020). "Chloroquine". StatPearls. Treasure Island (FL): StatPearls Publishing LLC. PMID 31855356.
- "Medicines for the Prevention of Malaria While Traveling – Chloroquine (Aralen)" (PDF) (Fact sheet). U.S. Centers for Disease Control and Prevention (CDC).
 The dictionary definition of chloroquine at Wiktionary
The dictionary definition of chloroquine at Wiktionary